Urinary Tract Infections: Uncomplicated
Authors: FME Wagenlehner, MD, PhD, KG Naber, MD, PhD
BACKGROUND
Acute, uncomplicated UTIs in adults include episodes of acute cystitis and acute pyelonephritis occurring in otherwise healthy individuals. These UTIs are seen mostly in women who have no risk factors, i.e. no structural or functional abnormalities within the urinary tract and the kidneys and no underlying disease known to increase the risks of acquiring infection or of failing therapy. Uncomplicated UTIs are extremely common infections. Approximately 25-35% of women between the ages of 20 and 40 years have experienced an episode described by their physician as an uncomplicated UTI.
DEFINITION
The distinction between an uncomplicated and a complicated UTI is important because of implications with regard to pre- and post-treatment evaluation, the type and duration of antimicrobial regimens, and the extent of the evaluation of the urinary tract. In contrast to an uncomplicated UTI, a complicated UTI is an infection associated with a condition that increases the risks of acquiring an infection or of failing therapy. At the time of presentation with an acute onset of urinary tract symptoms, it is usually not possible to classify definitively patients as having a complicated or an uncomplicated UTI. Several factors have been identified, however, that are markers for a potential complicated UTI:
- Male sex
- Elderly
- Hospital-acquired infection
- Pregnancy
- Indwelling urinary catheter
- Recent urinary tract intervention
- Functional or anatomical abnormality of the urinary tract
- Recent antimicrobial use
- Symptoms for > 7 days at presentation
- Diabetes mellitus
- Immunosuppression
These factors only provide guidance to the clinician who must decide, based on limited clinical information, whether to embark on a more extensive evaluation and treatment course. It is generally safe to assume that a pre-menopausal, non-pregnant woman with acute onset of dysuria, frequency or urgency, who has not recently been instrumented or treated with antimicrobials and who has no history of a genitourinary tract abnormality, has an uncomplicated lower (cystitis) or upper (pyelonephritis) UTI. Recurrent UTIs are common among pre-menopausal, sexually active, healthy women, even though they generally have anatomically and physiologically normal urinary tracts. Whether a UTI in pregnancy by itself is to be classified as an uncomplicated or a complicated UTI remains debatable. Although data on UTIs in healthy post-menopausal women without genitourinary abnormalities are limited, it is likely that most UTIs in such women are also uncomplicated. Data on UTIs in healthy adult men are sparse and much less is known about the optimal diagnostic and therapeutic approaches to UTIs in men.
ETIOLOGICAL SPECTRUM
The spectrum of etiological agents is similar in uncomplicated upper and lower UTIs, with E. coli being the causative pathogen in approximately 70-95% of cases and Staphylococcus saprophyticus in about 5-19% of cases, whereas S. saprophyticus is less frequently found in pyelonephritis than in cystitis. Occasionally, other Enterobacteriaceae, such as P. mirabilis and Klebsiella spp., or enterococci (mostly in mixed cultures indicating contamination), are isolated from such patients. In as many as 10-15% of symptomatic patients, bacteriuria cannot be detected using routine methods.
ACUTE UNCOMPLICATED CYSTITIS IN PRE-MENOPAUSAL, NON-PREGNANT WOMEN
At this stage in life, the incidence of acute uncomplicated cystitis is high and this infection is associated with considerable morbidity. Therefore, even small improvements in diagnostics, therapy or prophylaxis have a high impact on public health.
Incidence, Risk Factors, Morbidity
A prospective study at a university health centre or a health maintenance organization (HMO) revealed an incidence of 0.7 per person-year in the university cohort and 0.5 per person-year in the HMO cohort. Cohort and case control studies in young women showed that the risk is strongly and independently associated with recent sexual intercourse, recent use of diaphragm with spermicide, preceding asymptomatic bacteriuria, a history of recurrent UTI, the age of first UTI and history of UTI in the mother. On average, each episode of this type of UTI in pre-menopausal women was shown to be associated with 6.1 days of symptoms, 2.4 days of restricted activity, 1.2 days in which they were not able to attend classes or work and 0.4 days in bed.
Diagnosis
A non-pregnant pre-menopausal woman presenting with acute dysuria usually has one of three types of infection:
- acute cystitis
- acute urethritis, caused by Chlamydia trachomatis, Neisseria gonorrhoeae, or herpes simplex virus
- vaginitis caused by Candida spp. or Trichomonas vaginalis.
A distinction between these three entities can usually be made with a high degree of certainty from the history and physical examination.
Acute cystitis is more likely if the woman complains of urgency and suprapubic pain; has suprapubic tenderness; is a diaphragm-spermicide user; has symptoms that mimic those of previously confirmed cystitis; or has recently undergone urethral instrumentation. Although approximately 40% of women with cystitis have haematuria, this is not a predictor of a complicated infection. Urethritis caused by N. gonorrhoeae or C. trachomatis is relatively more likely if a women has had a new sexual partner in the past few weeks or if her sexual partner has urethral symptoms; there is a past history of a sexually transmitted disease (STD); symptoms were of gradual onset over several weeks and there are accompanying vaginal symptoms such as vaginal discharge or odour. Vaginitis is suggested by the presence of vaginal discharge or odour, pruritus, dyspareunia, external dysuria and no increased frequency or urgency.
Urinalysis (e.g. using a dipstick method) to look for pyuria, haematuria and nitrites is indicated if a UTI is suspected. Pyuria is present in almost all women with an acutely symptomatic UTI and in most women with urethritis caused by N. gonorrhoeae or C. trachomatis; its absence strongly suggests an alternative diagnosis. The definitive diagnosis of a UTI is made in the presence of significant bacteriuria, the definition of which remains somewhat controversial. The traditional standard for significant bacteriuria is ≥ 105 cfu uropathogen/mL in voided mid-stream sample of urine, based on studies of women with acute pyelonephritis and asymptomatic bacteriuria that were carried out four decades ago. Several more recent studies have shown that this is an insensitive standard when applied to acutely symptomatic women and that approximately one-third to one-half of cases of acute cystitis have bacteriuria < 105 cfu/mL. For practical purposes, colony counts ≥ 103sub> cfu/mL should be used for the diagnosis of acute uncomplicated cystitis (Table 4). Sterile pyuria is defined as the presence of leukocytes without bacteria. The determination of a urine culture is generally not necessary in women with uncomplicated cystitis because the causative organisms and their antimicrobial susceptibility profiles are predictable. Also, culture results become available only after the patient’s symptoms have resolved or are considerably improved. Voided mid-stream sample of urine or straight catheter (by trained urological personnel) urine cultures should probably be performed if the patient’s symptoms are not characteristic of a UTI. The laboratory must be instructed to look for ‘low count’ bacteriuria if such UTIs are to be detected. A pelvic examination is indicated if any of the factors suggesting urethritis or vaginitis listed above are present or if there is doubt as to the diagnosis. A pelvic examination should include a careful evaluation for evidence of vaginitis, urethral discharge, or herpetic ulcerations; a cervical examination for evidence of cervicitis and cervical and urethral cultures for N. gonorrhoeae and C. trachomatis (or other sensitive and specific tests in first-voided urine in the morning, such as polymerase chain reaction tests).
Treatment
There seems to be no long-term adverse effects with respect to renal function or increased mortality associated with acute uncomplicated cystitis, even in women who experience frequent recurrences, and in the non-pregnant population. Untreated cystitis rarely progresses to symptomatic upper tract infection. Thus, the significance of lower tract infection in non-pregnant women seems to be limited to the morbidity of symptoms caused by the infection, which can lead to substantial disruption of the lives of affected individuals. In fact, most lower UTIs (50-70%) clear spontaneously if untreated, although symptoms may persist for several months. Knowledge of the antimicrobial susceptibility profile of uropathogens causing uncomplicated UTIs in the community should guide therapeutic decisions. The resistance pattern of E. coli strains causing an uncomplicated UTI, however, may vary considerably between regions and countries. Short courses of antimicrobials are highly effective in the treatment of acute uncomplicated cystitis in pre-menopausal women (Table 1). Short-course regimens are desirable because of the improved compliance that they promote, their lower cost, and lower frequency of adverse reactions. However, in assessing the potential cost advantages of short-course regimens, it is necessary to consider the potential added expense associated with treatment failures or recurrences arising from short-course therapy. It is also important to consider the potential psychological aspects of single-dose therapy; as symptoms may not subside for 2 or 3 days, the patient may have misgivings during this time about the ‘insufficient’ treatment provided to her. Such a scenario may result in unnecessary visits or calls to the physician.
The following antimicrobial agents can be used for treatment of uncomplicated cystitis: trimethoprim (TMP), trimethoprim-sulfamethoxazole (TMP-SMX), fluoroquinolones (ciprofloxacin, enoxacin, fleroxacin, gatifloxacin, levofloxacin, lomefloxacin, norfloxacin, ofloxacin, pefloxacin, rufloxacin), ß-lactams (amoxicillin, ampicillin-like compounds, cefadroxil, cefuroxime axetil, cefpodoxime proxetil, ceftibuten, pivmecillinam, ritipenem axetil), fosfomycin trometamol, and nitrofurantoin (Table 1).
The following conclusions about antimicrobial therapy can be made:
Treatment Duration
In otherwise healthy, adult, non-pregnant women with acute uncomplicated cystitis, single-dose therapy (with some exceptions) is significantly less effective in eradicating initial bacteriuria than are longer durations of treatment with antimicrobials tested in this manner, such as TMP-SMX, TMP, norfloxacin, ciprofloxacin, fleroxacin, and as a group ß-lactams. However, TMP-SMX, TMP, norfloxacin, ciprofloxacin, and fleroxacin given for 3 days are as effective as the same antimicrobials used over longer durations. Longer treatment usually shows a higher rate of adverse events.
Trimethoprim, Co-trimoxazole
A 3-day regimen with TMP-SMX can be considered to be the standard therapy. TMP alone was equivalent to TMP-SMX with regard to eradication and adverse effects. Considering possible rare, but serious, adverse effects caused by sulphonamides, TMP alone may be considered the preferred drug over TMP-SMX. TMP or TMP-SMX can be recommended as first-line drugs for empirical therapy, but only in communities with rates of uropathogen resistance to TMP < 10-20% because there is a close correlation between susceptibility and the eradication of E. coli on the one hand and resistance and persistence of the uropathogen on the other. The risk of emerging resistant uropathogens in the case of recurrence was also much higher when using TMP as a first-line drug than when using pivmecillinam or ciprofloxacin, which had the lowest risk of the drugs investigated.
Fluoroquinolones
The fluoroquinolones (ciprofloxacin, fleroxacin, norfloxacin and ofloxacin) are equivalent to TMP-SMX when given as a 3-day regimen. Pefloxacin and rufloxacin, each as single-day therapies, are interesting options and may be equivalent to TMP-SMX in the eradication of bacteriuria and its recurrence. Questions remain as to the possibility of a higher incidence of adverse effects with these agents than with other recommended therapies. A 3-day regimen with levofloxacin, 250 mg once daily, was similarly effective to a 3-day regimen of ofloxacin 200 mg twice daily, but with levofloxacin there was a trend to lesser adverse events. A 3-day course with CiproXR (500 mg) once daily was equivalent inregard to efficacy and safety as a course of conventional ciprofloxacin (250 mg twice daily).
Fluoroquinolones are more expensive than TMP and TMP-SMX, and are thus not recommended as first-line drugs for empirical therapy except in communities with rates of uropathogen resistance to TMP > 10-20%. In some countries, however, the resistance of E. coli to fluoroquinolones has already increased to more than 10%. In this situation, alternative oral drugs should be considered for empirical therapy. Treatment with any of these agents should result in more than 90% eradication of the bacteriuria.
ß-lactam Antibiotics
In general, ß-lactams as a group are less effective than the aforementioned drugs. First- and second-generation oral cephalosporines are not recommended as first-line antimicrobials for a 3-day treatment of uncomplicated UTI. However, among third-generation oral cephalosporins, a 3-day course with cefpodoxime-proxetil (200 mg twice daily) was as safe and effective as that of TMP-SMX. One exception might be pivmecillinam. 7 days of pivmecillinam, 200 mg twice daily, was equivalent to 3 days of norfloxacin, 400 mg twice daily. With pivmecillinam, however, the rate of vaginal candidiasis was significantly lower than with norfloxacin. Pivmecillinam also shows low resistance rates for E. coli and other Enterobacteriaceae, without cross-resistance to other antimicrobials used for the treatment of UTI.
Fosfomycin
Single dose fosfomycin trometamol (3 g) therapy has shown good results regarding bacteriological eradication. Considering that fosfomycin trometamol has been extensively used in several European countries for single-dose therapy of uncomplicated UTI since 1988, the resistance rate for E. coli remained very low without cross-resistance to other antimicrobials used for the treatment of UTI.
Nitrofurantoin
Nitrofurantoin (50-100 mg four times daily, or sustained release formulation 100 mg twice daily) cannot be considered a suitable drug for short-term therapy (up to 3 days) of acute uncomplicated cystitis. A course of 5-7 days is recommended if nitrofurantoin is used for this indication. Despite the clinical use of nitrofurantoin for many years, the resistance rate for E. coli and S. saprophyticus is still low throughout Europe, although in some areas a two-fold increase in nitrofurantoin resistance has already been observed for E. coli within the last 10 years. Nitrofurantoin is, however, not active against P. mirabilis and Klebsiella spp., the second and third most frequently isolated Gram-negative uropathogens. There is also some concern about the safety of nitrofurantoin, especially the acute and chronic pulmonary syndromes, which are common in the elderly. These severe adverse events, however, were not observed when nitrofurantoin was used for long-term and low-dose prophylaxis for recurrent UTIs in girls and women.
Other Treatment Modalities
Urinary analgesics, such as phenazopyridine, 200 mg three times daily, can be administered to patients who have experienced severe dysuria for 1 or 2 days. Women with cystitis, including those with severe dysuria and urgency, usually show resolution or marked improvement of symptoms within 2-3 days of initiating therapy. This should be explained to the patient. Thus, the need for, and duration of, analgesic therapy in women with UTIs must be individualized. Although it is generally recommended that patients with UTIs increase their fluid intake to promote micturition and the elimination of uropathogens, it remains unclear as to whether this is beneficial or detrimental to patients with UTI.
Post-treatment Follow-up
Urinalysis (e.g using a dipstick method) is sufficient for routine follow-up. Routine post-treatment cultures in asymptomatic patients may not be indicated because the benefit of detecting and treating asymptomatic bacteriuria in healthy women has been demonstrated only in pregnancy and prior to urological instrumentation or surgery. In women whose symptoms do not resolve by the end of treatment and in those whose symptoms resolve but recur within 2 weeks, urine culture and antimicrobial susceptibility testing should be performed. For therapy in this situation, one should assume that the infecting organism is not susceptible to the agent originally used and retreatment with a 7-day regimen using another agent should be considered.![]()
ACUTE UNCOMPLICATED PYELONEPHRITIS IN PRE-MENOPAUSAL, NON-PREGNANT WOMEN
Diagnosis
Acute pyelonephritis is suggested by flank pain, nausea and vomiting, fever (> 38°C), or costovertebral angle tenderness, and may occur with or without cystitis symptoms. The presentation of an acute uncomplicated pyelonephritis usually varies from a mild to a moderate illness. A life-threatening condition with multi-organ system dysfunction, including sepsis syndrome with or without shock and renal failure, must be considered a complicated case. Urinalysis is indicated to look for pyuria and haematuria. In contrast to cystitis, 80-95% of episodes of pyelonephritis are associated with > 105 cfu uropathogen/mL. For routine diagnosis, a breakpoint of 104 cfu/mL can be recommended (Table 4). An evaluation of the upper urinary tract with ultrasound should be performed to rule out urinary obstruction. Additional investigations, such as an unenhanced helical computed tomography (to rule out urolithiasis), an excretory urogram or DMSA scan, according to the clinical situation should be considered if the patient remains febrile after 72 hours of treatment to rule out further complicating factors, e.g. urolithiasis, renal or perinephric abscesses. Routine performance of an excretory urogram in patients with acute uncomplicated pyelonephritis has little value because most adults with uncomplicated acute pyelonephritis have a normal upper urinary tract.
Treatment
The following aspects should be considered for treatment (Table 2):
1. TMP-SMX is preferred over ampicillin.
2. Two weeks of therapy with TMP-SMX for acute uncomplicated pyelonephritis appears to be adequate for the majority of women.
3. In communities in which the resistance rate of E. coli to TMP is > 10%, a fluoroquinolone should be recommended as the drug of choice for empirical therapy. It was demonstrated that a 7-day regimen of ciprofloxacin, 500 mg twice daily, showed a significantly higher rate of bacterial eradication and a lower rate of adverse effects when compared with a 14-day therapy using TMP-SMX, 960 mg twice daily. The following fluoroquinolones are also comparable to conventional ciprofloxacin 500 mg twice daily: ciprofloxacin extended release formulation (1000 mg once daily), gatifloxacin (400 mg once daily), levofloxacin (250 mg twice daily), and lomefloxacin (400 mg once daily).
4. A 10-day therapy with cefpodoxime proxetil 200 mg twice daily is probably equivalent with ciprofloxacin 500 mg twice daily.
5. In areas with a rate of E. coli resistance to fluoroquinolones > 10% and in situations in which fluoroquinolones are contraindicated (e.g. pregnancy, lactating women, adolescence), an aminopenicillin plus a beta-lactamase inhibitor, or a group three oral cephalosporin is recommended, either for initial use, or if a patient has to be switched to an oral regimen.
Therefore in mild and moderate cases an oral fluoroquinolone could be used for 7 days as first-line therapy. In situations where a fluoroquinolone is not indicated, a group three oral cephalosporin, e.g. cefpodoxime proxetil, may be an alternative for empirical therapy. More severe cases of acute uncomplicated pyelonephritis should be admitted to hospital and, if the patient cannot take oral medication, treated parenterally with a fluoroquinolone, an aminopenicillin plus a beta-lactamase inhibitor, a group three cephalosporin, or an aminoglycoside. With improvement, the patient can be switched to an oral regimen using one of the above-mentioned antibacterials (if active against the infecting organism) to complete the 1-2 weeks’ course of therapy.
Although approximately 12% of patients hospitalized with acute uncomplicated pyelonephritis have bacteraemia, it is common practice to obtain blood cultures only if the patient appears ill enough to warrant hospitalization. There is no evidence that bacteraemia has prognostic significance or warrants longer therapy in an otherwise healthy individual with pyelonephritis.
Post-treatment Follow-up
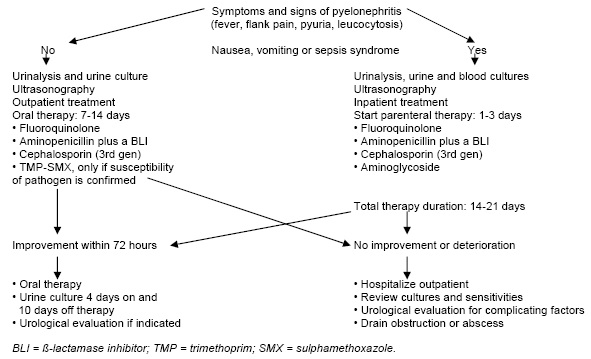
Routine post-treatment cultures in an asymptomatic patient may not be indicated; routine urinalysis using a dipstick method is sufficient. In women whose pyelonephritis symptoms do not improve within 3 days, or that resolve and then recur within 2 weeks, a repeat urine culture, antimicrobial susceptibility testing and an appropriate investigation, such as renal ultrasound or scan, should be performed. In the patient with no urological abnormality, it should be assumed that the infecting organism is not susceptible to the agent originally used and retreatment with a 2-week regimen using another agent should be considered. For those patients who relapse with the same pathogen as the initially infecting strain, a 6-week regimen is usually curative. An overview of the clinical management of acute pyelonephritis is shown in Figure 1.
RECURRENT (UNCOMPLICATED) UTIs IN WOMEN
Background
Recurrent urinary tract infection is defined in the literature by three episodes of UTI in the last 12 months or two episodes in the last 6 months. Risk factors for recurrent urinary tract infection are genetic and behavioural. Some studies estimate that 20-30% of women who have a UTI will have a recurrent urinary tract infection. Women who are non-secretors of blood group substances have an increased occurrence of recurrent urinary tract infection. A secretor is defined as a person who secretes their blood type antigens into body fluids and secretions, such as saliva, etc. A non-secretor on the other hand puts little to none of their blood type antigens into these fluids. In the USA about 20% of the population are non-secretors. Women with recurrent urinary tract infection have an increased frequency of urinary infection in first-degree female relatives. In addition, E. coli, the most common uropathogen, adheres more readily to epithelial cells in women who experience recurrent urinary tract infection. Behavioural factors associated with recurrent urinary tract infection include sexual activity, with a particularly high risk in those who use spermicides as a birth control method. According to cohort and case control studies, risk factors associated with recurrent urinary tract infection in sexually active premenopausal women are frequency of sexual intercourse, spermicide use, age of first UTI (less than 15 years of age indicates a greater risk of recurrent urinary tract infection) and history of UTI in the mother, suggesting that genetic factors and/or long-term environmental exposures might predispose to this condition. Following the menopause, risk factors strongly associated with recurrent urinary tract infection are vesical prolapse, incontinence and post-voiding residual urine. Other risk factors such as blood group substance non-secretor status and a history of UTI before the menopause need to be confirmed by further research.
Recurrent UTIs result in significant discomfort for women and have a high impact on ambulatory health care costs as a result of outpatient visits, diagnostic tests and prescriptions. Different approaches have been proposed for the prevention of recurrent urinary tract infection, including non-pharmacological therapies, such as voiding after sexual intercourse or the ingestion of cranberry juice, and the use of antibiotics as preventive therapy given regularly or postcoital prophylaxis in sexually active women.
With respect to antibiotic prophylaxis, it is not known which antibiotic schedule is best or the optimal duration of prophylaxis, the incidence of adverse events, or the recurrence of infections after stopped prophylaxis or treatment compliance.
Prophylactic Antimicrobial Regimens
One effective approach for the management of recurrent uncomplicated UTI is the prevention of infection through the use of long-term, prophylactic antimicrobials taken on a regular basis at bedtime or postcoital. Generally, the number of patients with microbiological recurrent UTIs decreased by eightfold as compared to the period of time before prophylaxis and compared to placebo by fivefold. The UTI episodes per patient-year is reduced in general by 95% during antimicrobial prophylaxis as compared to the period of time before prophylaxis. The duration of prophylactic therapy usually extends between 6 months or 1 year. Prophylaxis does not appear to modify the natural history of a recurrent UTI. When discontinued, even after extended periods, approximately 60% of women will become re-infected within 3-4 months.
The recommendations for antimicrobial regimens for the prevention (prophylaxis) of recurrent uncomplicated UTI in pre-menopausal women are listed in Table 3. Trimethoprim, co-trimoxazole or nitrofurantoin can still be considered as the standard regimen. Fosfomycin trometamol (FT), 3g every 10 days for 6 months can be considered as an alternative. An alternative prophylactic approach is post-intercourse prophylaxis for women in whom episodes of infection are associated with sexual intercourse. Generally, for this approach, the same antimicrobials can be used in the same doses as though recommended for continuous prophylaxis. A patient-initiated treatment may also be suitable for management in well-informed, young women, in whom the rate of recurrent episodes is not too common. This is, however, strictly speaking, not prophylaxis but early treatment.
UTI's IN PREGNANCY
Urinary tract infections are common during pregnancy. There is some debate about whether these infections can be classified as uncomplicated, even in cases where no further risk factors besides pregnancy can be found. Bearing this in mind, the three entities, asymptomatic bacteriuria, acute cystitis and acute pyelonephritis, will be discussed in this section with regard only to pregnancy and not to other risk factors.
The factors that predispose a woman to UTI in pregnancy appear to be related to the anatomical and physiological changes in the kidney and urinary tract that occur during pregnancy. The ureters become dilated above the pelvic brim and the bladder is displaced anteriorly and superiorly by the enlarging uterus. Renal blood flow and the glomerular filtration rate increase by about 30-40% during pregnancy and the kidneys become slightly enlarged and hyperaemic. Urine flow may be sluggish and the bladder may not empty completely.
Epidemiology
The prevalence of asymptomatic bacteriuria in American, European and Australian studies varies between 4% and 7%. Incidence relates to sexual activity and increases with increasing age and gravidity. It is also higher among patients from lower socio-economic groups. Symptomatic infection occurs in about 1-2% of pregnant women.
Most women acquire bacteriuria before pregnancy. At the first examination, the rates of bacteriuria in pregnant women are similar to those in non-pregnant women with similar risk factors. About 37-57% of bacteriuric schoolgirls develop UTIs during pregnancy. An additional 1% of infections occur during pregnancy. Bacteriuria during pregnancy is associated with a significant increase in the number of low-birth-weight infants (< 2500 g), low gestational age (< 37 weeks), and neonatal mortality. Women with persistent infection despite treatment or with evidence of ‘tissue invasion’ are at a higher risk of delivering premature infants. It should, however, be mentioned that bacterial vaginosis is also an important independent risk factor for premature birth; hence, treatment is recommended.
Asymptomatic Bacteriuria
Early studies by Kass and others demonstrated that 20-40% of women with asymptomatic bacteriuria develop pyelonephritis during pregnancy. Treatment of the bacteriuria lowers this risk. It is therefore generally recommended that pregnant women should be screened for bacteriuria by urine culture at least once in early pregnancy, and they should be treated if results are positive. To avoid unnecessary treatment, asymptomatic bacteriuria is defined as two consecutive positive cultures of the same species. The false-positive rate of a single mid-stream sample of urine may be as high as 40%. Therefore, women with a positive urine culture should be asked to return within 1-2 weeks, at which time, after stressing the importance of a careful cleansing of the vulva before micturition, a second mid-stream sample of urine or straight catheter urine specimen is obtained for culture. Treatment should be based on antibiotic sensitivity testing and usually involves a 5- to 7-day course of antibiotics. Follow-up cultures should be obtained 1-4 weeks after treatment and at least once more before delivery.
Acute Cystitis During Pregnancy
Most symptomatic UTIs in pregnant women present as acute cystitis, as occurs in non-pregnant women. Usually a 7-day treatment course is recommended, e.g. with pivmecillinam. Short-term therapy is not as established in pregnant women as it is in non-pregnant women, but it is recommended by smaller studies and expert opinion. Fosfomycin trometamol (3 g single dose) or second- and third generation oral cephalosporins (e.g. ceftibuten 400 mg once daily) could be considered candidates for effective short-term therapy. Otherwise conventional therapy with amoxicillin, cephalexin or nitrofurantoin is recommended.
Follow-up urine cultures should be obtained after therapy to demonstrate eradication of the bacteriuria. As in non-pregnant women, there is no advantage to be gained by using long-term prophylaxis except for recurrent infections. Low-dose cephalexin (125-250 mg) or nitrofurantoin (50 mg) at night are recommended for prophylaxis against re-infection if indicated, lasting up to and including the puerperium. Postcoital prophylaxis may be an alternative approach.
Acute Pyelonephritis in Pregnancy
Acute pyelonephritis tends to occur during the later stages of pregnancy, usually in the last trimester. The incidence of acute pyelonephritis in obstetric patients is 2%. The incidence is increased in the puerperium. Characteristically, the patient is acutely ill with high fever, leucocytosis and costovertebral angle pain. Bacteraemia is common, but mortality and complications are low when the patient is treated with effective therapy. The major causes of concern are the presence of underlying urological abnormalities and associated risks to the mother and fetus, such as toxaemia, hypertension, prematurity and perinatal mortality. Currently, antimicrobial therapy is so effective that, even with bacteraemia, almost all patients with uncomplicated pyelonephritis do well and become afebrile within a few days. Recommended antibiotics include second- or third-generation cephalosporins, an aminopenicillin plus a BLI, or an aminoglycoside. During pregnancy, quinolones, tetracyclines and TMP should not be used during the first trimester, while sulphonamides should not be used in the last trimester. In cases of delayed defeverescence and upper tract dilatation, a ureteral stent may be indicated and antimicrobial prophylaxis until delivery and including the puerperium should be considered.
UTIs IN POST-MENOPAUSAL WOMEN
The normal vagina contains only low numbers of Gram-negative enteric bacteria because of competition from the resident microbial flora. Lactobacilli account for the low vaginal pH. They tend to be less abundant in postmenopausal women and after antimicrobial therapy. Oestrogens are presumed to exert a protective force against recurrent UTIs in post-menopausal women because they enhance the growth of lactobacilli and decrease vaginal pH. Gram-negative enteric bacteria do not ordinarily colonize the vagina in postmenopausal women unless these women are prone to recurrent UTIs. In post-menopausal women with recurrent UTIs, therapy with oral or intravaginal oestriol reduced significantly the rate of recurrence. For other patients, an antimicrobial prophylactic regimen should be recommended in addition to hormonal treatment. In the case of an acute UTI, the antimicrobial treatment policy is similar to that in pre-menopausal women. Short-term therapy in post-menopausal women is not, however, as well documented as in younger women.
ACUTE UNCOMPLICATED UTIs IN YOUNG MEN
Pathogenesis and Risk Factors
It has been conventional to consider all UTIs in men as complicated because most UTIs occurring in the newborn, infant or elderly male are associated with urological abnormalities, bladder outlet obstruction or instrumentation. A UTI in an otherwise healthy adult man between the ages of 15 and 50 years is very uncommon. The large difference in the prevalence of UTIs between men and women is thought to be caused by a variety of factors, including the greater distance between the usual source of uropathogens (the anus and the urethral meatus); the drier environment surrounding the male urethra; the greater length of the male urethra; and the antibacterial activity of the prostatic fluid. It has become clear, however, that a small number of men aged 15-50 years suffer acute uncomplicated UTIs. The exact reasons for such infections are not clear, but risk factors associated with such infections include intercourse with an infected partner, anal intercourse and lack of circumcision; however, these factors are not always present. More than 90% of men with febrile UTI (fever > 38.0°C), with or without clinical symptoms of pyelonephritis, have a concomitant infection of the prostate, as measured by transient increases in serum PSA and prostate volume, irrespective of prostatic tenderness.
Diagnosis (Table 4)
The symptoms of uncomplicated UTIs in men are similar to those in women. Urethritis must be ruled out in sexually active men using a urethral Gram stain or a first-voided urine specimen wet mount to look for urethral leucocytosis. A urethral gram stain demonstrating leucocytes and predominant Gram-negative rods suggests E. coliurethritis, which may precede or accompany a UTI. Dysuria is common to both UTI and urethritis. The eetiological agents that cause uncomplicated UTIs in men are also similar to those in women.
Treatment (Table 5)
Empirical use of the agents discussed previously for uncomplicated cystitis or pyelonephritis in women are recommended. Nitrofurantoin should not be used in men with a UTI, since it does not achieve reliable tissue concentrations. For acute uncomplicated pyelonephritis, the use of a fluoroquinolone as initial empirical treatment is recommended in areas where the rate of E. coli resistance to fluoroquinolones is low (< 10%). Otherwise, alternative drugs have to be considered. Since in most men with febrile UTI or pyelonephritis, prostatic involvement also has to be considered, the goal of treatment is not only to sterilize the urine, but also to eradicate the prostatic infection. Thus, antimicrobials with good prostatic tissue and fluid penetration are preferable, e.g. fluoroquinolones.
A minimum of 7 days of therapy is recommended, because of the relatively greater likelihood of an occult complicating factor in men compared with women. Urological evaluation should be carried out routinely in adolescents and in men with febrile UTI, pyelonephritis and recurrent infections, or whenever a complicating factor is present.
ASYMPTOMATIC BACTERIURIA
Asymptomatic bacteriuria is common. Populations with structural or functional abnormalities of the genitourinary tract may have an exceedingly high prevalence of bacteriuria, but even healthy individuals frequently have positive urine cultures. Asymptomatic bacteriuria is seldom associated with adverse outcomes.
Pregnant women and individuals undergoing traumatic genitourinary interventions are at risk for complications of bacteriuria and show benefit from screening and treatment programmes. Screening for or treatment of asymptomatic bacteriuria is not recommended for the following persons:
- pre-menopausal, non-pregnant women
- diabetic women
- older persons living in community
- elderly institutionalized subjects
- persons with spinal cord injury
- catheterized patients while the catheter remains in situ.
In fact, treatment of bacteriuria may be associated with harmful outcomes, such as increased shortterm frequency of symptomatic infection, adverse drug effects, and re-infection with organisms of increased antimicrobial resistance. Screening for asymptomatic bacteriuria and treatment is recommended only for selected groups where benefit has been shown:
- pregnant women
- before transurethral resection of the prostate and other traumatic urological interventions.
Antimicrobial therapy should be initiated before the procedure. Short-term antimicrobial treatment of asymptomatic women with catheter-acquired bacteriuria that persists 48 hours after removal of the indwelling catheter may be considered.
References
1. Brumfitt W, Hamilton-Miller JM. Efficacy and safety profile of long-term nitrofurantoin in urinary tract infections: 18 years’ experience. J Antimicrob Chemother 1998;42:363-371. [PubMed]
2. Hamm M, Wawroschek F, Weckermann D, Knopfle E, Hackel T, Hauser H, Krawczak G, Harzmann R. Unenhanced helical computed tomography in the evaluation of acute flank pain. Eur Urol 2001;39:460-465. [PubMed]
3. Hooton TM. Fluoroquinolones and resistance in the treatment ofuncomplicated urinary tract infection. Int J Antimicr Agents 2003;22(Suppl 2):65-72. [PubMed]
4. Hooton TM, Scholes D, Hughes JP, Winter C, Roberts PL, Stapleton AE, Stergachis A, Stamm WE. A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med 1996;335:468-474. [PubMed]
5. Hooton TM, Scholes D, Stapleton AE, Roberts PL, Winter C, Gupta K, Samadpour M, Stamm WE. A prospective study of asymptomatic bacteriuria in sexually active young women. N Engl J Med 2000;343:992-997. [PubMed]
6. Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am 1997;11:551-581. [PubMed]
7. Hooton TM, Winter C, Tiu F, Stamm WE. Randomized comparative trial and cost analysis of 3-day antimicrobial regimens for treatment of acute cystitis in women. JAMA 1995;273:41-45. [PubMed]
8. Kahlmeter G; ECO.SENS. An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections: the ECO.SENS Project. J Antimicrob Chemother 2003; 51:69-76. [PubMed]
9. Lecomte F, Allaert FA. Single-dose treatment of cystitis with fosfomycin trometamol (Monuril): analysis of 15 comparative trials on 2.048 patients. Giorn It Ost Gin 1997;19:399-404.
10. Naber KG. Short-term therapy of acute uncomplicated cystitis. Curr Opin Urol 1999;9:57-64. [PubMed]
11. Naber KG, Allin DM, Clarysse L, Haworth DA, James IG, Raini C, Schneider H, Wall A, Weitz P, Hopkins G, Ankel-Fuchs D. Gatifloxacin 400 mg as a single shot or 200 mg once daily for 3 days is as effective as ciprofloxacin 250 mg twice daily for the treatment of patients with uncomplicated urinary tract infections. Int J Antimicrob Agents. 2004;23:596-605. [PubMed]
12. Naber KG, Bartnicki A, Bischoff W, Hanus M, Milutinovic S, van Belle F, Schonwald S, Weitz P, Ankel- Fuchs D. Gatifloxacin 200 mg or 400 mg once daily is as effective as ciprofloxacin 500 mg twice daily for the treatment of patients with acute pyelonephritis or complicated urinary tract infections. Int J Antimicrob Agents 2004;23(Suppl 1):41-53. [PubMed]
13. Naber KG, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Grabe M, Lobel B, Palou J, Tenke P. EAU guidelines on the management of urinary and male genital tract infections. EAU Working Group on Urinary and Male Genital Tract Infections. European Association of Urology (EAU) Guidelines Office. 2006 edition. 1-126.
14. Nicolle LE. Asymptomatic bacteriuria: when to screen and when to treat. Infect Dis Clin North Am 2003;17:367-394. [PubMed]
15. Nicolle LE. Pivmecillinam in the treatment of urinary tract infections. J Antimicrob Chemother 2000;46(Suppl 1):35-39. [PubMed]
16. Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM; Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005;40:643-654. [PubMed]
17. Nicolle LE, Harding GK, Preiksaitis J, Ronald AR. The association of urinary tract infection with sexual intercourse. J Infect Dis 1982;146:579-583. [PubMed]
18. Pfau A. Recurrent UTI in pregnancy. Infection 1994;22(Suppl 1):49. [PubMed]
19. Raz R, Gennesin Y, Wasser J, Stoler Z, Rosenfeld S, Rottensterich E, Stamm WE. Recurrent urinary tract infections in postmenopausal women. Clin Infect Dis. 2000;30:152-156. [PubMed]
20. Schaeffer AJ, Jones J, Dunn JK. Association of vitro Escherichia coli adherence to vaginal and buccal epithelial cells with susceptibility of women to recurrent urinary-tract infections. N Engl J Med 1981;304:1062-1066. [PubMed]
21. Talan DA, Klimberg IW, Nicolle LE, Song J, Kowalsky SF, Church DA. Once daily, extended release ciprofloxacin for complicated urinary tract infections and acute uncomplicated pyelonephritis. J Urol 2004;171:734-739. [PubMed]
22. Talan DA, Stamm WE, Hooton TM, Moran GJ, Burke T, Iravani A, Reuning-Scherer J, Church DA. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis in women: a randomized trial. JAMA 2000;283:1583-1590. [PubMed]
23. Vosti KL. Recurrent urinary tract infections. Prevention by prophylactic antibiotics after sexual intercourse. JAMA 1975;231:934-940. [PubMed]
24. Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis 1999;29:745-758. [PubMed]
25. Weidner W, Ludwig M, Weimar B, Rau W. Rational diagnostic steps in acute pyelonephritis with special reference to ultrasonography and computed tomography scan. Int J Antimicrob Agents 1999;11:257-259. [PubMed]
Table 1. Recommended Antimicrobial Regimens for the Treatment of Acute Uncomplicated Bacterial Cystitis in Adult Premenopausal, Non-pregnant Women
| Substance | Dosage | Duration |
|---|---|---|
| Cefpodoxime | 100 mg bid | 3 days |
| Ciprofloxacin* | 250 mg bid | 3 days |
| CiproXR* | 500 mg od | 3 days |
| Fosfomycin trometamol | 3000 mg SD | 1 day |
| Levofloxacin* | 250 mg od | 3 days |
| Nitrofurantoin | 50-100 mg tid, | 5-7 days |
| 100 mg SR bid | ||
| Norfloxacin* | 400 mg bid | 3 days |
| Ofloxacin* | 200 mg bid | 3 days |
| Pivmecillinam | 200 mg bid | 7 days |
| Trimethoprim (TMP)* | 200 mg bid | 5-7 days |
| TMP-SMX* | 160/800 mg bid | 3 days |
| *Resistance rates of E.coli vary considerably within countries. These substances are only recommended for empirical therapy when the resistance rate of E. coli is < (10%-)20%. CiproXR = ciprofloxacin sustained release; SMX = sulphamethoxazole; od = once daily; bid = twice daily; qid = four times daily; SD = single dose; SR = sustained release. |
||
Table 2. Oral Treatment Options of Acute Uncomplicated Pyelonephritis in Adult Pre-menopausal Non-pregnant Women.
| Substance | Dosage | Duration |
|---|---|---|
| Ciprofloxacin | 500 mg bid | 7 days |
| CiproXR | 1000 mg od | 7-10 days |
| Cefpodoxime proxetil | 200 mg bid | 10 days |
| Gatifloxacin | 400 mg od | 10 days |
| Levofloxacin | 250 mg od | 10 days |
| Lomefloxacin | 400 mg od | 10 days |
| TMP-SMX | 160/800 mg bid | 14 days |
Table 3. Recommendations for Antimicrobial Prophylaxis of Recurrent Uncomplicated UTI in Women
Agent1 |
Dose |
|---|---|
Standard regimen: |
|
| • Nitrofurantoin | 50 mg/day |
| • Nitrofurantoin macrocrystals | 100 mg/day |
| • Trimethoprim-sulphamethoxazole | 40/200 mg/day or three times weekly |
| • Trimethoprim | 100 mg/day |
| • Fosfomycin trometamil | 3 g/10 day |
| ‘Breakthrough’ infections: | |
| • Ciprofloxacin | 125 mg/day |
| • Norfloxacin | 200-400 mg/day |
| • Pefloxacin | 800 mg/week |
| During pregnancy: | |
| • Cephalexin | 125 mg/day |
| • Cefaclor | 250 mg/day |
| 1 Taken at bedtime | |
Table 4. Criteria for The Diagnosis of A UTI, as Modified According to IDSA/ESCMID Guidelines
| Category | Description | Clinical features | Laboratory Investigations |
|---|---|---|---|
| 1 | Acute uncomplicated UTI Dysuria, in women; acute uncomplicated cystitis in women | urgency, frequency, suprapubic pain, no urinary symptoms in 4 weeks before this episode | ≥ 10 WBC/mm3 ≥ 103 cfu/mL* |
| 2 | Acute uncomplicated Fever, pyelonephritis | chills, flank pain; other diagnoses excluded; no history or clinical evidence of urological abnormalities (ultrasonography, radiography) | ≥ 10 WBC/mm3 ≥ 104 cfu/mL* |
| 3 | Complicated UTI | Any combination of symptoms from categories 1 and 2 above; one or more factors associated with a complicated UTI (see text) | ≥ 10 WBC/mm3 ≥ 105 cfu/mL* in women ≥ 104 cfu/mL* in men, or in straight catheter urine in women |
| 4 | Asymptomatic bacteriuria | No urinary symptoms | ≥ 10 WBC/mm3 ≥ 105 cfu/mL* in two consecutive MSU cultures ≥ 24 hours apart |
| 5 | Recurrent UTI (antimicrobial prophylaxis) | At least three episodes of uncomplicated infection documented by culture in last 12 months: women only; no structural/functional abnormalities | < 103 cfu/mL* |
| MSU = mid-stream sample of urine; UTI = urinary tract infection; WBC = white blood cells. All pyuria counts refer to unspun urine. *Uropathogen in MSU culture. | |||
Table 5. Recommendations for Antimicrobial Therapy in Urology
| Diagnosis | Most frequent pathogen/species | Initial, empirical antimicrobial therapy | Therapy duration |
|---|---|---|---|
| Cystitis acute, uncomplicated |
• E. coli • Klebsiella• Proteus• Staphylococci |
• Trimethoprim-sulphamethoxazole° | 3 days |
| • Fluoroquinolone* | (1-)3 days | ||
| • Fosfomycin trometamol | 1 day | ||
| • Pivmecillinam | (3-)7 days | ||
| • Nitrofurantoin | (5-)7 days | ||
| Pyelonephritis acute, uncomplicated | • E. coli• Proteus• Klebsiella• Other enterobacteria• Staphylococci |
• Fluoroquinolone*• Cephalosporin (group 3a)Alternatives:• Aminopenicillin/BLI• Aminoglycoside |
7-10 days |
UTI with complicating factors
Nosocomial UTIPyelonephritisacute, complicated |
• E. coli• Enterococci• Pseudomonas• Staphylococci• Klebsiella• Proteus• Enterobacter• Other enterobacteriav |
• Fluoroquinolone*• Aminopenicillin/BLI• Cephalosporin (group 2)• Cephalosporin (group 3a)• AminoglycosideIn case of failure of initial therapy within 1-3 days or in clinically severe cases:Anti-Pseudomonas active:• Fluoroquinolone, if not used initially• Acylaminopenicillin/BLI• Cephalosporin (group 3b)• Carbapenem• ± Aminoglycoside |
3-5 days after defeverescence or control/elimination of complicating factor
|
| • (Candida)
|
• Fluconazole• Amphotericin B |
||
| Prostatitis acute, chronic |
• E. coli• Other enterobacteria• Pseudomonas |
Fluoroquinolone*Alternative in acute bacterial prostatitis:• Cephalosporin (group 3a/b) |
Acute:
2-4 weeksChronic:4-6 weeks or longer |
| Epididymitis acute |
• Enterococci• Staphylococci• Chlamydia• Ureaplasma |
In case of Chlamydia or Ureaplasma:• Doxycycline• Macrolide |
10 days |
| Urosepsis | • E. coli• Other enterobacteriaAfter urological interventions – multi-resistant pathogens:• Pseudomonas• Proteus• Serratia• Enterobacter |
• Cephalosporin (group 3a/b)• Fluoroquinolone*• Anti-Pseudomonas active acylaminopenicillin/BLI• Carbapenem• Aminoglycoside |
3-5 days after defeverescence or control/elimination of complicating factor |
| BLI = ß-lactamase inhibitor; UTI = urinary tract infection. *Fluoroquinolone with mainly renal excretion (see text). °Only in areas with resistance rate < 20% (for E. coli). | |||
Figure 1. Clinical Management of Acute Pyelonephritis
Usta TA. et al. Comparison of single-dose and multiple-dose antibiotics for lower urinary tract infection in pregnancy. Int J Gynaecol Obstet. 2011 Sep;114(3):229-33.
Stapleton AE, et al. Randomized, Placebo-Controlled Phase 2 Trial of a Lactobacillus crispatus Probiotic Given Intravaginally for Prevention of Recurrent Urinary Tract Infection. Clinical Infectious Diseases. 2011;52(10):1212-7.
Falagas ME, Kastoris AC, et al. Fosfomycin for the Treatment of Multidrug-Resistant, Including Extended-Spectrum beta-Lactamase Producing, Enterobacteriaceae Infections: A Systematic Review. Lancet Infect Dis. 2010 Jan;10:43-50.
Talan DA, et al. Prevalence and Risk Factor Analysis of Trimethoprim-Sulfamethoxazole and Fluoroquinolone-Resistant Escherichia coli Infection among Emergency Department Patients with Pyelonephritis. Clinical Infectious Diseases 2008;47:1150–1158.
Koeijers JJ, Kessels AG, Nys S, Bartelds A, Donker G, Stobberingh EE, Verbon A. Evaluation of the nitrite and leukocyte esterase activity tests for the diagnosis of acute symptomatic urinary tract infection in men. Clin Infect Dis 2007;45:894-896.
GUIDED MEDLINE SEARCH FOR
López-Medrano F, María Aguado J. Urinary Tract Infections in Transplant Recipients
Gupta K, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of American and the European Society for Microbiology and Infectious Diseases. Clin infect Dis 2011;52(5) e103-20.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Clin Infect Dis 2005;40:643-654.
GUIDED MEDLINE SEARCH FOR RECENT REVIEWS
GUIDED MEDLINE SEARCH FOR HISTORICAL ASPECTS
Table of Contents
- Background
- Definition
- Etiological Spectrum
- Acute Uncomplicated Cystitis in Pre-menopausal, Non-pregnant Women
- Acute Uncomplicated Pyelonephritis in Pre-Menopausal, Non-Pregnant Women
- Recurrent (Uncomplicated Utis in Women)
- Uti's in Pregnancy
- Utis in Post-Menopausal Women
- Acute Uncomplicated Utis in Young Men
- Asymptomatic Bacteriuria
