|
Sample |
Laboratory studies |
|
Serum |
Blood cultures |
|
|
CMV quantitative viral load by PCR |
|
|
Aspergillus galactomannen antigen |
|
|
Histoplasma, Cryptococcus, Blastomycosisantibody titer |
|
|
Histoplasma, Cryptococcus antigen |
|
|
|
|
Urine |
Pneumococcal antigen |
|
|
Legionella antigen |
|
|
Histoplasmaantigen |
|
|
|
|
Nasopharyngeal swab or sputum |
Routine culture and Gram stain |
|
|
Fungal culture and stain |
|
|
AFB culture and stain |
|
|
Viral antigen testing for RSV, parainfluenza, influenza, adenovirus |
Table 2: Radiographic signs associated with microbiological diagnoses
|
Finding |
Suspected pathogen |
|
Focal consolidation |
Bacterial pathogens |
|
"Tree-in-bud opacity" |
Atypical pathogens including fungi and mycobacteria |
|
Ground glass opacity |
P. jiroveci, viral infections including CMV in at-risk patients |
|
Nodular opacity |
Fungi and mycobacteria |
|
"Halo sign" |
Aspergillus |
|
Pneumothorax |
P. jiroveci |
Table 3: Laboratory evaluation of bronchoalveolar lavage (BAL) samples
|
Essential studies |
· Gram stain and quantitative culture · Fungal evaluation (wet mount stain and culture) · Mycobacterial evaluation (AFB stain and culture) · Viral detection and culture (CMV, HSV, Adenovirus, RSV, Parainfluenza virus) · Gomori methamine silver stain or PCR for P. jiroveci |
|
Optional studies |
· Aspergillus galactomannan antigen · Nocardia culture · Actinomyces culture · Toxoplasmosis IFA/DFA |
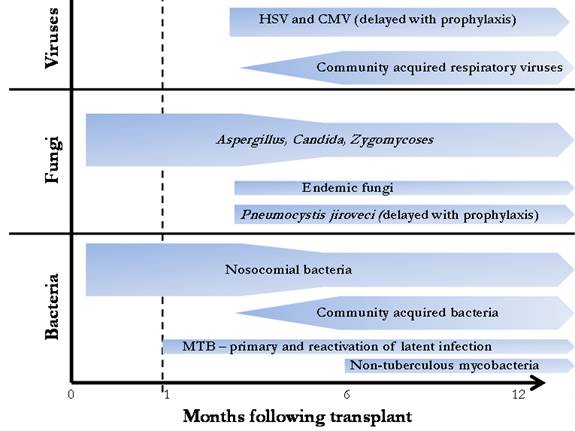
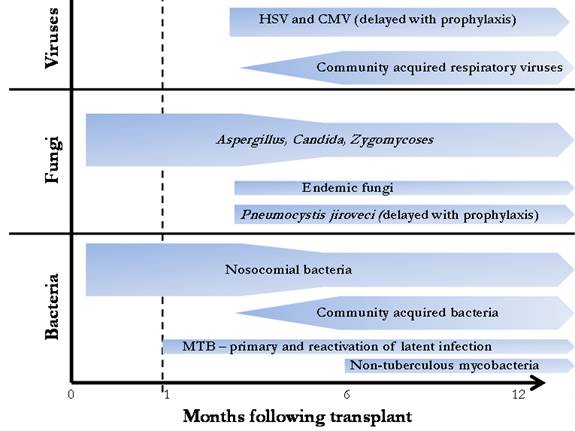
Temporal relationship between infectious etiology and time after transplantation. The risk for bacterial and fungal pneumonia is greatest in the first four weeks and decreases after three months, whereas the risk for CMV infection peaks after the discontinuation of antiviral prophylaxis in at-risk patients. Non-CMV viral infection is typically community acquired and develops more than 6 months after surgery.
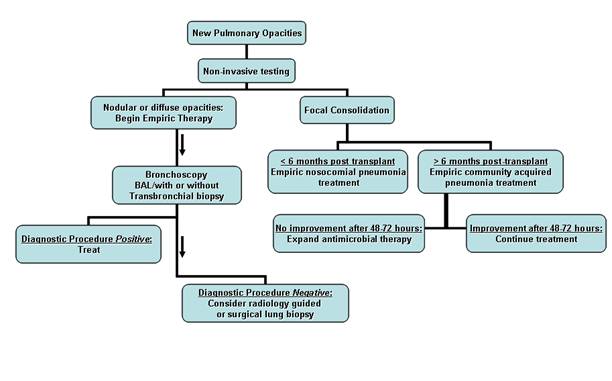
Suggested approach to suspected pneumonia in a solid organ transplant recipient. Focal radiographic consolidative changes in conjunction with findings suggestive of bacterial pneumonia lead to empiric antibiotic therapy. Patients presenting > 6 months after transplantation are treated for community acquired pneumonia with observation
while those < 6 months post-procedure are treated for nosocomial infection. All patients
in the latter category, lung transplant recipients, and those non-responsive to empiric therapy should have bronchoscopy performed. Patients with diffuse or nodular opacities should receive empiric treatment but bronchoscopy should be performed to obtain a diagnosis. In patients without a diagnosis after bronchoscopic evaluation, radiologic percutaneous biopsy or surgical lung biopsy should be considered.