Kikuchi-Fujimoto Disease (Histiocytic Necrotizing Lymphadenitis)
Authors: Paola Scagni, M.D., Ph.D.
GENERAL DESCRIPTION
Kikuchi-Fujimoto disease, also known as Kikuchi’s disease or histiocytic necrotizing lymphadenitis, is a benign, self-limiting cause of lymphadenopathy, variably associated with systemic symptoms. First described independently by Kikuchi (27) and Fujimoto (19) in 1972, Kikuchi-Fujimoto disease is increasingly recognized in the literature, but its true incidence is unknown.
Microbiology
The role of infectious agents in the pathogenesis and evolution of Kikuchi-Fujimoto disease is a matter of debate.
Epidemiology
Kikuchi-Fujimoto disease is an extremely rare disease known to have a worldwide distribution with a higher prevalence among Asiatic individual (4). Kikuchi-Fujimoto disease affects individuals of all ages, preferentially adult females under 30 years of age, but it has rarely been reported in children.(17, 31, 33, 47, 51, 61) This gender difference, with female predominance, has not been confirmed in more recent reports from Eastern countries and in pediatric studies.(4, 31, 33, 34, 35, 64).
Clinical Manifestations
The onset of Kikuchi-Fujimoto disease is acute or subacute, evolving over a period of two to four weeks. Clinically, the most common presentation is unilaterally lymphadenopathy with tenderness: cervical lymph nodes are the principle site of disease in 70-90% of patients; other lymph nodes, such as the axillary and abdominal ones, may be less frequently involved. Generalized adenopathy is uncommon.(11, 16, 17, 34, 47, 61). The size of affected lymph nodes is usually less than 4 cm and rarely larger than 6 cm. In addition to lymphadenopathy, 30-50% of patients have fever; (17, 31, 35) occasionally, Kikuchi-Fujimoto disease has been reported as a cause of prolonged fever of unknown origin (33). Parotidomegaly, with intragland lymphadenitis and hepatosplenomegalia may be present (4, 26, 32, 51). Less frequent symptoms include fatigue, arthralgia, night sweats, headache, myalgia, weight loss and gastroenteric complaints. Cutaneous involvement, like facial rash, exudative erythema and erythematous papules, is observed in 30-40 % of cases (31, 64, 65).
The outcome of the disease is usually favorable, with spontaneous resolution within a period of one to 6 months after diagnosis. There are occasional reports of unusual features of Kikuchi-Fujimoto disease (46), including severe extranodal involvement -such as myocarditis(48) and pulmonary hemorrhage(63)- and disseminated disease with fatal outcome (7, 29, 38).
A low recurrence rate has been described in 3% to 4% of cases (3, 16, 31, 34, 50, 61). Kikuchi-Fujimoto disease has been linked to systemic lupus erythematosus (SLE), as well as to other autoimmune diseases.(4, 8, 14, 18, 31, 34, 35). In particular, KLD and SLE may coexist with one preceding the other; this association is significantly high in cases from Eastern countries compared to cases from Europe (29). Other autoimmune connective tissue disorders, such as Still’s disease and primary Sjogren’s syndrome, have been described in association with SLE (13, 43, 53, 64). Post-transplantation development of Kikuchi-Fujimoto disease is a further interesting issue (60). Patients require a regular follow-up for several years to rule out the development of SLE.
Laboratory Diagnosis
No specific laboratory test is available for the diagnosis.
Leukopenia occurs in 30 to 70% of cases. Other nonspecific laboratory findings include anemia, atypical peripheral blood lymphocytes and increased erythrocyte sedimentation rate with low C-reactive protein values in most patients (30-50% of cases); serum hepatic transaminase activities and lactate dehydrogenase levels are also frequently increased (4, 34, 61, 64).
Diagnosis of Kikuchi-Fujimoto Disease
The diagnosis of Kikuchi-Fujimoto disease is based on the histological findings of affected lymph nodes. Due to partial lymph node involvement an excisional biopsy is mostly preferred, although fine needle aspiration biopsy sometimes may prove helpful (59, 62).
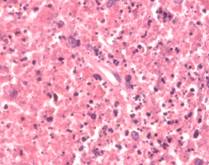
Typical histopathological features (Figure 1) include extensive fibrinoid necrosis, loss of lymph node architecture, absence of granulomatous reaction with foamy histiocytes at the margin of the necrotic areas. The karyorrhectic foci are formed by different cellular types, predominantly histiocytes and plasmacytoid monocytes, but also immunoblasts, some of which may be atypical, and small or large lymphocytes (4). Neutrophils are characteristically absent and plasma cells are either absent or scarce. Immunohistochemistry is an important tool for distinguishing Kikuchi-Fujimoto disease from lymphoma. The immunophenotype of Kikuchi-Fujimoto disease typically consists of a predominance of T cells, with prevalence of CD8+ expression over CD4+ cells. Relatively few B cells and NK cells are present. The histiocytes express histiocyte-associated antigens such as lysozyme, myeloperoxidase and CD68. Striking plasmacytoid monocytes are also positive for CD68 but not for myeloperoxidase (4, 31, 52).
Pathogenesis
Although the etiology of Kikuchi-Fujimoto disease remains unclear, infectious causes and autoimmune mechanisms have been alternatively suggested. Both the benign course and complete recovery of Kikuchi-Fujimoto disease seem to correlate with a self-limited infectious process. An autoimmune contribution to the pathogenesis is based on observations showing an association of Kikuchi-Fujimoto disease with systemic lupus erythematosus and other connective tissue disorders (16, 17, 34, 40).
Currently, the most favored theory proposes that Kikuchi-Fujimoto disease might represent an exuberant T-cell mediated immune response to a variety of non-specific stimuli in genetically susceptible individuals.(4, 17) To further suggest a genetic predisposition, some HLA class II genes have been more frequently observed in patients with Kikuchi-Fujimoto disease (58).
Due to histopathologic and clinical features of Kikuchi-Fujimoto disease, several lymphocyte-infecting viruses have been postulated to have a causative role. These include Epstein-Barr virus (EBV),(9, 11, 23, 54) cytomegalovirus (CMV),(23) parvovirus B19,(9, 42) human herpesvirus 6 (HHV-6),(10, 15, 21, 36, 39, 55) varicella-zoster virus, parainfluenza virus, human herpesvirus 7 (HHV-7),(10) human herpesvirus 8 (HHV-8) (10, 20, 24) and human T-cell lymphotrophic virus-1.(1, 9) So far, such investigations have produced conflicting results; most of the immunohistochemical and molecular studies failed to link Kikuchi-Fujimoto disease to specific pathogens or demonstrated that these viruses are no more common than in control patients.(9, 10, 20, 21, 39, 55) Therefore the role of virus in the pathogenesis and evolution of Kikuchi-Fujimoto disease remains controversial and not yet convincingly demonstrated.
Among bacteria and parasites, Yersinia enterocolitica, Brucella melitensis,(6) Toxoplasma gondii, Giardia lamblia (5) and Entamoeba histolytica (2) have been occasionally identified by serologic and cultural methods and have all been implicated in the pathogenesis, without any convincing corroborating evidence. Interestingly, gene products of Bartonella henselae have been recently detected in lymph nodes of children with Kikuchi-Fujimoto disease (12).
Although the mechanism of cell death involved in Kikuchi-Fujimoto disease has not been extensively studied, Ohshima et al (45) have shown that apoptotic cell death may play a role in the pathogenesis of the disease. According to these Authors, proliferating CD8 positive T-cells may act as “killers” and victims” in the apoptotic process via Fas- end perforine- pathways (45). Perforine, a killer cell-specific cytolytic protein essential for provoking apoptosis in target cells, has been reported to be expressed abundantly by infiltrating cytotoxic T lymphocytes. Therefore, the necrosis associated with Kikuchi-Fujimoto disease might be attributable to trans apoptotic death of the killer cell target in the affected nodes (57). Serum concentration of some inflammation mediators, such as interferon- and interleukin-6, have been reported to be increased during the acute phase of Kikuchi-Fujimoto disease, raising the possibility that these cytokines could have a role in the pathogenesis of this condition (28).
Differential Diagnosis
In terms of clinical and laboratory presentation, Kikuchi-Fujimoto disease could easily be confused with other infectious, reactive and lymphoproliferative diseases, such as tuberculosis, toxoplasmosis, mononucleosis, sarcoidosis, Kawasaki’s disease, SLE and non-Hodgkin's lymphoma (46).
Owing to the variable degree of microscopic necrosis found within the lymph nodes as well as the atypia in the reactive immunoblastic component, the histopathological appearances of Kikuchi-Fujimoto disease may be very similar to those found in other diseases, especially SLE and lymphoma (4). That confusion has led some patients to extensive and aggressive diagnostic evaluations and even unnecessary treatment (17, 41).
The presence of numerous plasma cells and hematoxylin bodies favors SLE-associated lymphadenitis over Kikuchi-Fujimoto disease(4, 17, 65). Immunohistochemistry is an important tool for distinguishing Kikuchi-Fujimoto disease from lymphoma.
SUSCEPTIBILITY IN VITRO AND IN VIVO
The relationship of Kikuchi-Fujimoto disease with infections is controversial; therefore no in vitro or animal studies on drug susceptibility exist.
ANTIMICROBIAL THERAPY
Given the lack of in vitro and animal data, sparse reports of empirical antibiotic treatment in humans constitute the only data available. These include successful responses to minocycline (56) and ciprofloxacin (37). Therapeutic response to antibiotics has been used as supportive evidence for an infective etiology in Kikuchi-Fujimoto disease. Recognizing the significant limitations of the above data, we do not recommend an antibiotic regimen. No antiviral therapy has been used in clinical practice.
Underlying Diseases
There is no evidence that Kikuchi-Fujimoto disease is more prevalent in immunocompromised patients, or that treatment should be modified in this population.
ADJUNCTIVE THERAPY
The course of Kikuchi-Fujimoto disease is typically benign and self-limited; no specific therapy has therefore been established for Kikuchi-Fujimoto disease.
Treatment is generally symptomatic and supportive: non-steroidal anti-inflammatory drugs and acetaminophen are beneficial in relieving distressing local and systemic complaints. Adjunctive therapy has been focused on patients with recurrent, generalized or severe disease in order to prevent a fatal outcome. The majority of reports are of treatment with corticosteroids (mainly prednisone), to which some patients seem to respond (22, 25, 33, 47). Glucocorticoids have also been applied to patients with prolonged fever unresponsive to initial non-steroidal anti-inflammatory drugs (25, 30, 47). Due to variable responseadditional studies are needed for validating steroid treatment for this disease (25).
Empirical treatment include hydroxychloroquine, successfully used in a patient with recurrent Kikuchi-Fujimoto disease (49). There is a single case report describing intravenous immunoglobulin treatment (0.4 g/kg per day for 3 days) in a patient with severe Kikuchi-Fujimoto disease (44). Excisional lymph node biopsy for the purpose of confirming the diagnosis is the only surgery indicated in Kikuchi-Fujimoto disease.
ENDPOINTS FOR MONITORING THERAPY
No therapeutic endpoints have been established. Cessation of fever and general malaise is usually the first objective signs of improvement, followed by reduction of lymph nodes. Laboratory and histologic abnormalities lag behind the clinical gains.
VACCINES
There are no experimental or commercially available vaccines for prevention of Kikuchi-Fujimoto disease.
PREVENTION OR INFECTION CONTROL MEASURES
Since the relation between Kikuchi-Fujimoto disease and infections remains a matter of debate, no special prevention or infection control measures are advised.
CONTROVERSIES, CAVEATS OR COMMENTS
Several questions are worthy of further investigations. Which is the role of infections in Kikuchi-Fujimoto disease? Which is the relation between Kikuchi-Fujimoto disease and autoimmune disorders? Should Kikuchi-Fujimoto disease be treated with glucocorticoids? Does antibiotic therapy provide any additional benefit in Kikuchi-Fujimoto disease therapy?
REFERENCES
1. Atarashi K, Yoshimura N, Nodera H, Tsukimoto K, Beppu H, Kanayama M. Recurrent histiocytic necrotizing lymphadenitis (Kikuchi disease) in an human T lymphotropic virus type I carrier. Intern Med 1996; 35:821-825 [PubMed]
2. Aydogan T, Kanbay M, Uraldi C, Kaya A, Uz B, Isik A, Akcay A, Erekul S. Kikuchi Fujimoto disease secondary to Entamoeba histolytica: case report. J Infect 2006; 53(4):e171-e173 [PubMed]
3. Blewitt RW, Kumar SN, Abraham JS. Recurrence of Kikuchi's lymphadenitis after 12 years. J Clin Pathol 2000;53:175-8 [PubMed]
4. Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol 2004; 122: 157-158 [PubMed]
5. Charalabopoulos K, Charalabopoulos A, Papadopoulou CH, Papalimneou V. Giardia lamblia intestinalis: a new pathogen with possible link to Kikuchi-Fujimoto disease. An additional element in the disease jigsaw. Int J Clin Pract 2004; 12:1180-1183 [PubMed]
6. Charalabopoulos K, Papalimneou V, Charalabopoulos A, Bai M, Agnantis N. Brucella melitensis infection stimulates an immune response leading to Kikuchi-Fujimoto disease. In vivo 2003; 17:51-53 [PubMed]
7. Chan JK, Wong KC, Ng CS. A fatal case of multicentric Kikuchi’s histiocytic necrotizing lymphadenitis. Cancer 1989; 63: 1856-1862 [PubMed]
8. Chen YH, Lan JL. Kikuchi disease in systemic lupus erythematosus: clinical features and literature review. J Microbiol Immunol Infect 1998; 31:187-192 [PubMed]
9. Chiu CF, Chow KC, Lin TY, Tsai MH, Shih CM, Chen LM. Virus infection in patients with histiocytic necrotizing lymphadenitis in Taiwan. Detection of Epstein-Barr virus, type I human T-cell lymphotropic virus, and parvovirus B19. Am J Clin Pathol 2000; 113(6):774-81 [PubMed]
10. Cho MS, Choi HJ, Park HK, Cho SE, Han WS, Yang WI. Questionable role of human herpesviruses in the pathogenesis of Kikuchi disease. Arch Pathol Lab Med 2007; 131: 604-609 [PubMed]
11. Cho KJ, Lee SS, Khang SK. Histiocytic necrotizing lymphadenitis. A clinico-pathologic study of 45 cases with in situ hybridization for Epstein-Barr virus and hepatitis B virus. J Korean Med Sci 1996;11(5):409-14.
12. Chung JY, Kim SW, Han TH, Lim SJ. Detection of the bartonella henselae gene sequence in lymph nodes of children with Kikuchi’s disease. Pediatrics 2005; 115:1112 [PubMed]
13. Cousin F, Grezard P, Roth B, Balme B, Gregoire-Bardel M, Perrot H. Kikuchi disease associated with Still disease. Int J Dermatol 1999; 38:464-467 [PubMed]
14. Dalkilic E, Karakoc Y, Tolunay S, Yurtkuran M. Systemic lupus erythematosus presenting as Kikuchi-Fujimoto disease. Clin Exp Rheumatol 2001; 19:226 [PubMed]
15. Dominquez DC, Torres ML, Antony S. Is human herpesvirus 6 linked to Kikuchi-Fujimoto disease? The importance of consistent molecular and serologic analysis. South Med J 2003; 96:226-233 [PubMed]
16. Dorfman RF. Histiocytic necrotizing lymphadenitis of Kikuchi and Fujimoto. Arch Pathol Lab Med 1987; 111:1026-1029 [PubMed]
17. Dorfman RF, Berry GJ. Kikuchi’s histiocytic necrotizing lymphadenitis: an analysis of 108 cases with emphasis on differential diagnosis. Semin Diagn Pathol 1988; 5:329-45 [PubMed]
18. El-Ramahi KM, Karrar A, Ali MA. Kikuchi disease and its association with systemic lupus erythematosus. Lupus 1994; 3:409-411 [PubMed]
19. Fujimoto Y, Kojima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis. Naika 1972; 30:920-7
20. George TI, Jones CD, Zehnder JL, Warnke RA, Dorfman RF. Lack of human herpesvirus 8 and Epstein-Barr virus in Kikuchi’s histiocytic necrotizing lymphadenitis. Human Pathol 2003; 34:130-135 [PubMed]
21. Hollingsworth HC, Peiper SC, Weiss LM, Raffeld M, Jaffe ES. An investigation of the viral pathogenesis of Kikuchi-Fujimoto disease. Lack of evidence for Epstein-Barr virus or human herpesvirus type 6 as the causative agents. Arch Pathol Lab Med. 1994; 118(2):134-40 [PubMed]
22. Hrycek A, Cieslik P, Szkrobka W, Pajak J. Kikuchi-Fujimoto disease: a case report. Rheumatol Int 2005; 26:179-181 [PubMed]
23. Huh J, Chi HS, Kim SS, Gong G. A study of the viral etiology of histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease). J Korean Med Sci 1998; 13(1):27-30. [PubMed]
24. Huh J, Kang GH, Gong G, Kim SS, Ro JY, Kim CW. Kaposi’s sarcoma-associated herpesvirus in Kikuchi’s disease. Hum Pathol 1998; 29:1091-1096 [PubMed]
25. Jang YJ, Park KH, Seok HJ. Management of Kikuchi’s disease using glucocorticoids. J Laryngol Otol 2000; 114:709-11 [PubMed]
26. Keogh MA, Williamson RM, Denaro CO. Kikuchi's disease associated with parotidomegaly, thyroiditis and a rash in a young man (letter). Aust N Z J Med. 2000;82:186-188 [PubMed]
27. Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes. Acta Haematol Jpn 1972; 35:379-80
28. Kubota M, Tsukamoto R, Kurokawa K, Imai T, Furushu K. Elevated serum interferon gamma and interleukin-6 in patients with necrotizing lymphadenitis (Kikuchi-Fujimoto disease). Br J Haematol 1996; 95:613-615 [PubMed]
29. Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M. Kikuchi-Fujimoto disease: analysis of 244 cases. Clin Rheumatol 2007; 26: 50-54 [PubMed]
30. Kumar TS, Scott JX, Agarwal I, Danda D. Management of Kikuchi disease using glucocorticoids. J Clin Rheumatol 2006; 12:47 [PubMed]
31. Kuo T. Kikuchi’s disease (histiocytic necrotizing lymphadenitis). A clinicopathologis study of 79 cases with an analysis of histologic subtypes, immunohistology and DNA ploidy. Am J Surg Pathol 1995;19:798-809. [PubMed]
32. Kuo T, Jung SM, Wu WJ. Kikuchi’s disease of intraparotid lymph nodes presenting as a parotid gland tumor with extranodal involvement of the salivary gland. Histopathology 1996; 28:185-188 [PubMed]
33. Lee KY, Yeon YH, Lee BC. Kikuchi-Fujimoto disease with prolonged fever in children. Pediatrics 2004; 114(6):e752:756 [PubMed]
34. Lin HC, Su CY, Huang CC, Hwhag CF, Chien CY. Kikuchi’s disease: a review and analysis of 61 cases.[PubMed] Otolaryngol Head Neck Surg 2003; 128:650-653 [PubMed]
35. Lin HC, Su CY, Huang SC. Kikuchi’s disease in Asian children. Pediatrics 2005 Jan;115(1):e92-e96 [PubMed]
36. Luppi M, Barozzi P, Garber R, Maiorana A, Bonacorsi G, Artusi T, Trovato R, Marasca R, Torelli G. Expression of human herpesvirus-6 antigens in benign and malignant lymphoproliferative diseases. Am J Pathol 1998; 153(3):815-23 [PubMed]
37. Mahajan VK, Sharma NL. Kikuchi Fujimoto disease: immediate remission with ciprofloxacin. Int J Dermatol 2004; 43(5):370-372 [PubMed]
38. Mahadeva U, Allport T, Bain B, Chan WK. Haemophagocytic syndrome and histiocytic necrotizing lymphadenitis (Kikuchi’s disease). J Clin Pathol 2000; 53:636-8 [PubMed]
39. Martinez-Vazquez C, Potel C, Angulo M, Gonzalez-Carrero J, Alvarez M, Tenorio A, Cid D, Oliveira I. Nosocomial Kikuchi's disease-a search for herpesvirus sequences in lymph node tissues using PCR. Infection 2001; 29(3):143-7 [PubMed]
40. Martinez-Vazquez C, Hughes G, Bordon J, Alonso-Alonso J, Anibarro-Garcia A, Redondo-Martinez E, Touza-Rey F. Histiocytic necrotizing lymphadenitis, Kikuchi-Fujimoto disease, associated with systemic lupus erythematosus. QJM 1997; 90: 531-533 [PubMed]
41. Menasce LP, Banerjee SS, Edmondson D. Histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease): continuing diagnostic difficulties Histopathology. 1998; 33:248-54 [PubMed]
42. Meyer O, Ribard P, Belmatoug N, Kahan MF, Grossin M, Fournet JC, Darne C, Morinet F. 3 cases of Kikuchi's lymphadenitis in systemic lupus erythematosus. Role of the parvovirus B19. Ann Med Interne 1991; 142:259-264 [PubMed]
43. Miyashita Y, Yamaguchi W, Fujimoto W. Painful indurated erythema suggestive of Kikuchi-Fujimoto disease in a patient with primary Sjogren’s syndrome. J Dermatol 2003; 30:608-611 [PubMed]
44. Noursadeghi M, Aqel N, Gibson P, Pasvol G. Successful treatment of severe Kikuchi’s disease with intravenous immunoglobulin. Rheumatology 2006; 45:235-237 [PubMed]
45. Ohshima K, Shimazaki K, Kume T, Suzumiya J, Kanda M, Kikuchi M. Perforin and Fas pathways of cytotoxic T-cells in histiocytic necrotizing lymphadenitis. Histopathology 1998; 33:471-478 [PubMed]
46. Onciu M; Medeiros LJ. Kikuchi-Fujimoto lymphadenitis. Adv Anat Pathol. 2003; 10: 204-211 [PubMed]
47. Park HS, Sung MJ, Park SE, Lim YT. Kikuchi-Fujimoto disease of 16 children in a single center of Korea. Pediatr Allergy Immunol 2007; 18:174-178 [PubMed]
48. Quintas-Cardama A, Fraga M, Cozzi SN, Caparrini A, Maceiras F, Forteza J. Fatal Kikuchi-Fujimoto disease: the lupus connection. Ann Hematol 2003; 82:186-188 [PubMed]
49. Rezai K, Kuchipudi S, Chundi V, Ariga R, Loew J, Sha BE. Kikuchi Fujimoto disease: hydroxychloroquine as a treatment. Clin Infect Dis 2004: 39:e124-e126 [PubMed]
50. Sah SK, Pant R, Piper K, Chowdhury TA, Crean SJ. Recurrent Kikuchi Fujimoto disease: Case report. Br J Oral Maxillofac Surg 2007; 45: 231-233 [PubMed]
51. Scagni P, Peisino MG, Bianchi M, Morello M, Sardi N, Linari A, Mastrodicasa L, Madon E, Pecco P. Kikuchi-Fujimoto disease is a rare cause of lymphadenopathy and fever of unknown origin in children: report of two cases and review of the literature. J Pediatr Hematol Oncol. 2005; 27:337-40. [PubMed]
52. Somech R, Leider-Trejo L, Assia A, Jurgenson U, Spirer Z. Kikuchi-Fujimoto disease: a rare presentation in a child and update review of the literature. Acta Pediatr 2002; 91:1402 [PubMed]
53. Soy M, Peynirci H, Bilgi S, Adali MK, Guresci S. Kikuchi-Fujimoto disease coexisted with Sjogren’s syndrome. Clin Rheumatol 2007; 26:607-608 [PubMed]
54. Stephan JL, Jeannoel P, Chanoz J, Gentil-Perret A. Epstein-Barr virus-associated Kikuchi disease in two children. J Pediatr Hematol Oncol. 2001; 23(4):240-3. [PubMed]
55. Sumiyoshi Y, Kiluchi M, Ohshima K, Yoneda S, Kobazi S, Takeshita M, Eizuru Y, Minamishima Y. Human herpesvirus-6 genomes in histiocytic necrotizing lymphadenitis (Kikuchi's disease) and other forms of lymphadenitis. Am J Clin Pathol 1993; 99(5):609-14. [PubMed]
56. Takada K, Suzuki K, Hidaka T, Konishi T, Shinohara T, Kataharada K, Matsumoto M, Okada M, Ohsuzu F. Immediate remission obtained by minocycline in a patient with histiocytic necrotizing lymphadenitis. Intern Med 2001; 40:1055-1058 [PubMed]
57. Takakuwa T, Ohnuma S, Koike J, Hoshikawa M, Koizumi H. Involvement of cell-mediated killing in apoptosis in histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease). Histopathology 1996; 28:41.48 [PubMed]
58. Tanaka T, Ohomori M, Yasunaga S. DNA typing of HLA class II genes (HLA- DR, -DQ and -DP) in Japanese patients with histiocytes necrotizing lymphadenitis (Kikuchi’s disease). Tissue Antigens 1999; 54:246-253 [PubMed]
59. Tong TR, Chan OW, Lee KC. Diagnosing Kikuchi disease in fine needle aspiration biopsy: a retrospective study of 44 cases diagnosed by cytology and 8 by histopathology. Acta Cytol 2001; 45:953-957 [PubMed]
60. Tsai MK, Huang HF, Hu RH, Lee PH, Lee CJ, Chao SH, Hsu HC, Ko WJ, Chu SH. Fatal Kikuchi-Fujimoto disease in transplant recipients: a case report. Transplant Proc 1998; 30:3137-3138 [PubMed]
61. Tsang WY, Chan JK, Ng CS. Kikuchi’s lymphadenitis. A morphologic analysis of 75 cases with special reference to unusual features. Am J Surg Pathol 1994; 18:219-231
62. Viguer JM, Jimenez-Heffernan JA, Perez P, Lopez-Ferrer P, Gonzales-Peramato P, Vicandi B. Fine-needle aspiration cytology of Kikuchi’s lymphadenitis: a report of ten cases. Diagn Cytopathol 2001; 25:220-224 [PubMed]
63. Wong CY, Law GT, Shum TT, Wong KY, Li YK. Pulmonary haemorrhage in a patient with Kikuchi disease. Monaldi Arch Chest Dis 2001; 56:118-120 [PubMed]
64. Wang TJ, Yang YH, Lin YT ; Chiang BL. Kikuchi-Fujimoto disease in children: clinical features and disease course. J Microbiol Immunol Infect 2004; 37:219-224[PubMed]
65. Yen HR, Lin PY, Chuang WY, Chang ML, Chiu CH. Skin manifestation of Kikuchi-Fujimoto disease: case report and review. Eur J Pediatr 2004; 163:210-13 [PubMed]
GUIDED MEDLINE SEARCH FOR:
GUIDED MEDLINE SEARCH FOR RECENT REVIEWS
GUIDED MEDLINE SEARCH FOR HISTORICAL ASPECTS
Kikuchi-Fujimoto Disease (Histiocytic Necrotizing Lymphadenitis)
Table of Contents
- General Description
- Microbiology
- Epidemiology
- Clincal Manifestations
- Laboratory Diagnosis
- Diagnosis of Kikuchi-Fujimoto Disease
- Pathogenesis
- Differential Diagnosis
- Susceptibility In Vitro and In Vivo
- Antimicrobial Therapy
- Adjunctive Therapy
- Endpoints for Monitoring Therapy
- Vaccines
- Prevention or Infection Control Measures
- Controversies, Caveats, or Comments