![]() Reprinted from
www.antimicrobe.org
Reprinted from
www.antimicrobe.org
Patient with Fever and Rash - Six Skin Rash Categories
PETECHIAE/PURPURA
There are life-threatening infections that present with petechiae/purpura so knowledge of this differential is critical for designing empiric antimicrobial therapy (Table 4). Sepsis of any etiology can be complicated by disseminated intravascular coagulation (DIC), vascular invasion and occlusion by organisms, immune vasculitis with immune complex deposition, embolic phenomena, or vascular effects of toxins. All of these mechanisms can contribute to the development of petechiae/purpura, therefore petechiae and purpura can be present in the absence of DIC.
Table 4. Infections Associated with Petechiae/Purpura Neisseria meningitidis
Rickettsia rickettsii
Streptococcus pneumoniae with asplenia
Capnocytophaga canimorsus with asplenia
Staphylococcus aureus endocarditis
Enteroviruses
Epstein - Barr virus
Hemorrhagic fever group of viruses
Patients with asplenia are at increased risk for overwhelming infection with Neisseria meningitidis, but even in normal hosts infection with this organism can present as fever and petechial rash. These patients usually have a rapidly progressive course with systemic toxicity. Central nervous system involvement may or may not be present. Organisms may be visible on skin biopsy but blood cultures are usually positive and are the best means of diagnosis. Empiric antimicrobial therapy should be started as soon as possible in the patient with suspected meningococcemia. Hospitalized patients should be placed on droplet precautions until they have received 24 hours of effective antimicrobial therapy. Lumbar puncture should be performed if the clinical picture is consistent with meningitis. Antibiotics should be started after blood has been obtained for culture but should not be delayed until spinal fluid is obtained. Neisseria meningitidis is sensitive to penicillin or ampicillin but ceftriaxone is often used in view of its superior penetration into the central nervous system. Prophylactic antibiotics are administered to close contacts of confirmed cases to prevent secondary cases.
A similar clinical picture can be seen in patients with Rocky Mountain spotted fever (RMSF), which is caused by Rickettsia rickettsii. Patients present with abrupt onset of high fever and severe frontal headache within a week of a bite from an infected tick. The rash usually appears after the fever and initially may be maculopapular, becoming more petechial as the illness progresses. The rash starts on the extremities, including the palms and soles, and spreads centrally. The season is an important consideration as RMSF presents in the spring and early summer. Travel history is also vital as RMSF is acquired most commonly in the southern Atlantic and the south central states. Not all patients recall a tick bite. If the time of the year and exposure history is consistent with RMSF empiric therapy with doxycycline 100mg po/ iv q 12 hours should be used to treat the patient with fever and a petechial rash. Untreated RMSF has a case fatality rate of 25 %. Rash may be absent in approximately 15 % of patients with RMSF. There are no routinely available rapid diagnostic tests for RMSF. The organism can not be grown in standard blood culture systems. Immunofluorescent staining of skin biopsy or four fold rise in IgG titers in serial serum specimens can be diagnostic but is not useful in acute management.
Patients with
functional or anatomic asplenia are at increased risk for sepsis with
encapsulated bacteria and are predisposed to the development of coagulopathy and
purpuric lesions
![]() during bacteremia. Encapsulated organisms including
Streptococcus pneumoniae, other streptococcal species,
Neisseria meningitides, and Haemophilus influenzae are the most
common etiologies. In asplenic patients with a history of dog exposure Capnocytophaga canimorsus should also be considered. Empiric therapy should
be started as soon as possible. A third generation cephalosporin, such as
ceftriaxone, can be used to treat all of the above. If the frequency of
penicillin resistance in Streptococcus pneumoniae is high in your
community vancomycin may be added.
during bacteremia. Encapsulated organisms including
Streptococcus pneumoniae, other streptococcal species,
Neisseria meningitides, and Haemophilus influenzae are the most
common etiologies. In asplenic patients with a history of dog exposure Capnocytophaga canimorsus should also be considered. Empiric therapy should
be started as soon as possible. A third generation cephalosporin, such as
ceftriaxone, can be used to treat all of the above. If the frequency of
penicillin resistance in Streptococcus pneumoniae is high in your
community vancomycin may be added.
Patients with acute endocarditis, usually secondary to Staphylococcus aureus, can also present with a toxic picture with fever and a petechial or purpuric rash. A history of pre-existing valvular heart disease may or may not be present. A history of active intravenous drug use or a new or changing murmur on physical exam may also raise the suspicion for this entity. Empiric therapy should be started after blood cultures have been obtained. Nafcillin is the drug of choice but vancomycin may be substituted if the patient has a severe penicillin allergy or if the prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in your community is significant (Figure 1).
Figure 1. Approach to Patient with Petechial Rash
|
52 year old asplenic patient with pneumococcal sepsis and purpura fulminans secondary to pneumonia. |
||||
|
|
|
|
|
|
There are a variety of non-treatable infections that can present with fever and petechial rash. Many common viruses, such as enteroviruses and Epstein-Barr virus (EBV), can cause a petechial rash as part of a systemic febrile illness. Enterovirus infections are discussed in the section on maculopapular rash. Epstein-Barr virus infections occur more frequently in children and young adults and present as a mononucleosis type syndrome characterized by pharyngitis, fever, malaise, adenopathy, splenomegaly and hepatitis. A monospot test is positive in the majority of patients with acute EBV mononucleosis, but specific EBV serology is also available. The viruses of the viral hemorrhagic fever group can also cause fever and a petechial rash. Most of these viruses would only be a concern in patients that have been involved in overseas travel to specific locations. Dengue is the most widespread of these viruses. Lassa fever virus, Ebola virus, Marburg virus and Machupo virus have been associated with life-threatening infection and can be spread nosocomially. Therefore patients suspected of having one of these viruses should be placed in isolation and the CDC and the state health department should be contacted immediately. Diagnosis is made by serology and treatment is supportive.
The list of non-infectious entities that can present with fever and petechial rash is extremely long. Thrombotic thrombocytopenia purpura (TTP) and the systemic vasculitis syndromes are important considerations in the differential of the patient with fever and petechial/purpuric rash. The classic pentad of TTP includes fever, hemolytic anemia, thrombocytopenia, neurologic dysfunction and decreased renal function. Demonstration of vasculitis on skin biopsy is an important component in the diagnosis of the systemic vasculitis syndromes. Leukocytoclastic vasculitis can be seen with a variety of infections such as subacute bacterial endocarditis, HIV infection, and chronic active hepatitis. Drug induced vasculitis with fever can be seen with a variety of different medications including allopurinol, phenytoin, penicillin, sulfonamides, and thiazides. As treatment for some of these vasculitic syndromes may require corticosteroids or other immunosuppressive medications it is important to rule out active infection first.
ERYTHEMA
The major infectious syndromes that present with fever and diffuse erythema
![]() (a) are
associated with specific toxins produced by the organisms (Table 5). Scarlet
fever results from infection with a strain of streptococcus that elaborates
streptococcal pyrogenic exotoxin. It is usually associated with pharyngitis but
it can occur following streptococcal infections at other sites. The erythroderma
is more pronounced in the skin folds ( Pastia's Lines) and there is circumoral
pallor. The classic oral manifestation is the strawberry tongue, which can
appear white or beefy red with prominent papillae. The rash is followed by
extensive desquamation. With extensive use of antimicrobial therapy for
streptococcal infections Scarlet fever has become uncommon. Staphylococcal Toxic
Shock Syndrome (STSS) occurs in patients who harbor strains of Staphylococcus
aureus that elaborate either toxic shock syndrome toxin 1 (TSST – 1) or
other related enterotoxins. Patients present with a syndrome of fever, diffuse
erythematous rash, hypotension and multisystem dysfunction. The mucous membranes
are often hyperemic and there is desquamation of the rash especially on the
palms and soles. Blood cultures and skin cultures are usually negative, but the
causative organism can be cultured from a colonized site. In addition to
aggressive supportive therapy patients are treated with an antistaphylococcal
antibiotic such as nafcillin. In the past there was an association of STSS with
the use of super absorbent tampons in women, but the majority of the recent
cases of Staphylococcal Toxic Shock Syndrome have been attributed to
non-menstrual sources. A similar toxic shock syndrome has been associated with
streptococcal infections. Group A beta-hemolytic streptococcus (GAS), or Streptococcus pyogenes, is the most common causative organism but other
streptococci can produce a similar clinical picture. In Streptococcal Toxic
Shock Syndrome the patients are usually bacteremic or have an active
streptococcal infection with the skin being the most common site. Patients
present with shock, fever, diffuse erythroderma and multiorgan failure.
Gastrointestinal symptoms of nausea, vomiting, and diarrhea may occur early in
the course of the illness. Pain at the site of infection precedes other signs of
infection such as erythema. Bullae may develop at the local site of infection
and the diffuse rash may desquamate during the convalescent phase of the
illness. Treatment includes aggressive supportive measures and empiric
antibiotic therapy effective against staphylococcus, streptococcus, anaerobes
and gram negative rods until a definitive diagnosis is made. Combination therapy
with penicillin and clindamycin is recommended for GAS.
(a) are
associated with specific toxins produced by the organisms (Table 5). Scarlet
fever results from infection with a strain of streptococcus that elaborates
streptococcal pyrogenic exotoxin. It is usually associated with pharyngitis but
it can occur following streptococcal infections at other sites. The erythroderma
is more pronounced in the skin folds ( Pastia's Lines) and there is circumoral
pallor. The classic oral manifestation is the strawberry tongue, which can
appear white or beefy red with prominent papillae. The rash is followed by
extensive desquamation. With extensive use of antimicrobial therapy for
streptococcal infections Scarlet fever has become uncommon. Staphylococcal Toxic
Shock Syndrome (STSS) occurs in patients who harbor strains of Staphylococcus
aureus that elaborate either toxic shock syndrome toxin 1 (TSST – 1) or
other related enterotoxins. Patients present with a syndrome of fever, diffuse
erythematous rash, hypotension and multisystem dysfunction. The mucous membranes
are often hyperemic and there is desquamation of the rash especially on the
palms and soles. Blood cultures and skin cultures are usually negative, but the
causative organism can be cultured from a colonized site. In addition to
aggressive supportive therapy patients are treated with an antistaphylococcal
antibiotic such as nafcillin. In the past there was an association of STSS with
the use of super absorbent tampons in women, but the majority of the recent
cases of Staphylococcal Toxic Shock Syndrome have been attributed to
non-menstrual sources. A similar toxic shock syndrome has been associated with
streptococcal infections. Group A beta-hemolytic streptococcus (GAS), or Streptococcus pyogenes, is the most common causative organism but other
streptococci can produce a similar clinical picture. In Streptococcal Toxic
Shock Syndrome the patients are usually bacteremic or have an active
streptococcal infection with the skin being the most common site. Patients
present with shock, fever, diffuse erythroderma and multiorgan failure.
Gastrointestinal symptoms of nausea, vomiting, and diarrhea may occur early in
the course of the illness. Pain at the site of infection precedes other signs of
infection such as erythema. Bullae may develop at the local site of infection
and the diffuse rash may desquamate during the convalescent phase of the
illness. Treatment includes aggressive supportive measures and empiric
antibiotic therapy effective against staphylococcus, streptococcus, anaerobes
and gram negative rods until a definitive diagnosis is made. Combination therapy
with penicillin and clindamycin is recommended for GAS.
Table 5. Illnesses Associated with Diffuse Erythema
Infectious Scarlet Fever Staphylococcal Toxic Shock Syndrome Streptococcal Toxic Shock Syndrome Arcanobacterium haemolyticum Staphylococcal Scalded Skin Syndrome Non-infectious Kawasaki Drug reaction Sezary
Infections resulting in more localized erythema may or may not be associated
with systemic symptoms such as fever. Staphylococcus aureus and beta
hemolytic streptococci are the most common causes of cellulitis, inflammation of
the dermis and subcutaneous tissue. The lower extremity is the most common site
for cellulitis but infection can occur at any site where pathogenic bacteria are
inoculated into the skin. Trauma and chronic edema of the extremity predispose
to the development of cellulitis. For example, patients with chronic edema of
the upper extremity following axillary lymph node dissection, or patients with
chronic edema following saphenous vein graft harvest are at increased risk for
developing cellulitis in the involved limbs. Cellulitis presents as a tender,
warm, erythematous and swollen area. There are indistinct borders to the
involved skin. Erysipelas is a superficial cellulitis with prominent lymphatic
involvement, resulting in induration with distinct borders and a peau d'orange
appearance to the skin. Bullae may complicate skin infections with both Staphylococcus aureus and beta hemolytic streptococci. Fever is often
present in patients with cellulitis or erysipelas. Blood cultures are positive
in a small percentage of cases and yield on culture of skin aspirate is low so
the diagnosis is usually clinical. These studies should not be performed
routinely and should be reserved for severe cases, immunocompromised patients,
or situations where there is increased suspicion for a resistant organism.
Patients should be treated with antibiotics effective for Staphylococcus
aureus and beta-hemolytic streptococci such as nafcillin or cefazolin.
Vancomycin may be used in patients with severe allergy to penicillin or if
Methicillin resistant Staphylococcus aureus (MRSA) is suspected.
Community acquired MRSA is becoming an increasing problem nation wide. Specific
exposure history may suggest other pathogens. Cellulitis following an animal
bite, especially a cat, is suggestive of Pasteurella multocida infection
![]() (b).
The treatment of choice for Pasteurella is amoxicillin-clavulanate, but a
quinolone can also be used.
(b).
The treatment of choice for Pasteurella is amoxicillin-clavulanate, but a
quinolone can also be used.
|
(a) Erythema: Redness that blanches with pressure |
(b) 35 year old with cellulitis and abscess after being scratched by a cat. An MRI revealed an abscess and tenosynovitis. Cultures were positive for Pasteurella multocida. |
|
 |
 |
 |
It is important to distinguish cellulitis from necrotizing soft tissue infections that can be seen with a variety of different pathogens. These infections often occur at sites of trauma or in areas with tissue hypoxia. Patients present with systemic toxicity and a rapidly progressive soft tissue infection. Patients complain of pain at the site that may seem out of proportion to the findings on physical examination. Bullae may develop and crepitus may be appreciated on physical examination. Plain radiographs may demonstrate air in the soft tissue. Necrotizing fasciitis can be seen with Streptococcus pyogenes infection but can also be polymicrobial (including anaerobes and gram negative bacilli). Myonecrosis secondary to Clostridium sps can present in a similar fashion. Surgical consultation should be obtained in patients where there is a suspicion for necrotizing soft tissue infection. Appropriate management includes aggressive supportive care, surgical debridement, and broad spectrum antibiotic therapy to cover GAS, anaerobes, and gram negative bacilli. Antimicrobial therapy can be tailored once results of blood and tissue cultures are available. The mortality even with appropriate therapy can be approximately 30 %.
Arcanobacterium haemolyticum can cause pharyngitis with diffuse erythroderma in young adults. The rash is localized to the trunk and the proximal upper extremities and does eventually desquamate with time. This organism is sensitive to a variety of antibiotics including tetracycline, erythromycin and clindamycin, but it may be tolerant to penicillin. A. haemolyticum may be missed on routine throat cultures.
In Staphylococcal Scalded Skin Syndrome (SSSS) patients present with fever and a scarlatiniform eruption. This is followed by the development of flaccid bullae, which result in denuded areas. These bullae tend to occur at sites of minor trauma (Nikolsky's sign) and the denuded areas eventually desquamate. This syndrome is a manifestation of infection with strains Staphylococcus aureus that produce an exfoliative exotoxin. Treatment includes supportive care and antimicrobial therapy effective for Staphylococcus aureus. Blood cultures may be positive, but skin biopsy is important to rule out Toxic Epidermal Necrolysis (TEN). Drugs are the most common etiology for TEN, which results in full thickness skin necrosis and a 10 – 30 % associated mortality.
Adverse reaction to medication can result in fever and rash. The classic drug rash is maculopapular but diffuse erythroderma can be seen, especially with sulfonamides or phenytoin. Kawasaki disease, or the mucocutaneous lymph node syndrome, is a systemic vasculitis that needs to be considered in the differential of a patient with fever and diffuse erythroderma. This disease is seen mostly in young children and occurs commonly in the late winter and spring. Patients present with fever, conjunctivitis, erythema of the oral mucosa and lips, rash, and cervical lymphadenopathy. The rash can be variable in appearance: scarlatiniform, pustular, plaque-like, or maculopapular. There is edema and erythema of the extremities including palms and soles, with subsequent desquamation starting in the periungual region. TSS secondary to Staphylococcus or streptococcus must be ruled out. Kawasaki syndrome can be complicated by cardiac involvement which is the major source of morbidity and mortality. Sezary syndrome, or cutaneous T cell lymphoma, can present with fever and diffuse erythroderma.
MACULES/PAPULES
The most common skin manifestation associated with infection is a maculopapular
rash
![]() (a). The differential diagnosis for fever and a maculopapular eruption is
extensive and includes many non-infectious entities. The typical drug reaction
that is seen seven to ten days into therapy is most commonly maculopapular in
character. The fever can precede the development of the rash, and both fever and
rash resolve after removal of the causative drug. The majority of infections
associated with fever and a maculopapular rash are viral
(a). The differential diagnosis for fever and a maculopapular eruption is
extensive and includes many non-infectious entities. The typical drug reaction
that is seen seven to ten days into therapy is most commonly maculopapular in
character. The fever can precede the development of the rash, and both fever and
rash resolve after removal of the causative drug. The majority of infections
associated with fever and a maculopapular rash are viral
![]() (b)
and are not treatable
(Table 6). With aggressive vaccine programs some of these infections have become
uncommon. Measles (rubeola) presents with fever, coryza and a maculopapular
rash, which starts in the head and neck region and spreads centrifugally. Mild
desquamation may occur. Early in the course of the illness small white spots,
Koplik's spots, are visible on the buccal mucosa opposite the lower molars. The
appearance is described as grains of sand embedded in the buccal mucosa.
Atypical measles can be seen in individuals that received the killed vaccine
between 1963 and 1967. The rash of atypical measles can be vesicular or purpuric
and starts on the extremities and spreads centrally. In individuals immunized
with the live virus vaccine protection wanes with time and mild measles can
occur in this population. Recognition of measles can be important as sporadic
cases do occur and it is associated with significant morbidity in
immunocompromised patients and in those at the extremes of age.
(b)
and are not treatable
(Table 6). With aggressive vaccine programs some of these infections have become
uncommon. Measles (rubeola) presents with fever, coryza and a maculopapular
rash, which starts in the head and neck region and spreads centrifugally. Mild
desquamation may occur. Early in the course of the illness small white spots,
Koplik's spots, are visible on the buccal mucosa opposite the lower molars. The
appearance is described as grains of sand embedded in the buccal mucosa.
Atypical measles can be seen in individuals that received the killed vaccine
between 1963 and 1967. The rash of atypical measles can be vesicular or purpuric
and starts on the extremities and spreads centrally. In individuals immunized
with the live virus vaccine protection wanes with time and mild measles can
occur in this population. Recognition of measles can be important as sporadic
cases do occur and it is associated with significant morbidity in
immunocompromised patients and in those at the extremes of age.
| (a) Macule: Flat discoloration < 1 cm in diameter | (a) Papule: Solid elevated lesion < 1 cm in diameter | |
|
|
|
|
|
(b) Patient with a macular rash from a presumed viral etiology |
||
|
|
|
|
Table 6. Infections Associated with Maculopapular Rash
| Rubella Virus (German Measles) | Ehrlichia and Anaplasma species (Ehrlichiosis) |
| Measles Virus (Rubeola) | Borrelia burgdorferi (Lyme disease) |
| Parvovirus B19 (Fifth Disease) | Dengue |
| Cytomegalovirus | Salmonella typhi (Typhoid Fever) |
| Primary HIV infection (Acute Retroviral Syndrome) | Rickettsia prowazekii (Louse-borne Typhus) |
| Epstein - Barr virus | Rickettsia typhi (Murine Typhus) |
| Human Herpesvirus-6 (Roseola) | Leptospira (Leptospirosis) |
| Enteroviruses | Chlamydia psittaci (Psittacosis) |
| Treponema pallidum (Secondary Syphilis) | Streptobacillus moniliformis (Rate-bite fever) |
| Rickettsia rickettsii (Rocky Mountain Spotted Fever) | Spirillum minus (Rate-bite fever) |
The maculopapular rash with Rubella begins on the face and spreads to cover most of the body. Patients have fever, malaise and posterior cervical lymphadenopathy. Petechiae may be visible on the soft palate and the rash may clear with mild desquamation. Recognition of Rubella may be especially important if a susceptible pregnant woman is exposed to a patient with fever and a maculopapular rash of unknown etiology. Congenital Rubella is associated with a large number of birth defects. Rubella can cause a significant arthritis in adults, especially women.
Fifth disease, or erythema infectiosum, is caused by Parvovirus B19. Children present with a classic slapped-cheek appearance followed by a more generalized maculopapular rash. The rash follows the febrile period in this illness and the rash may recur with various stimuli such as sun exposure. The papular-purpuric gloves and socks syndrome (PPGSS) is an unusual manifestation of Parvovirus B 19 infection. Patients with PPGSS develop painful and pruritic swelling and erythema of the distal extremities. Papular/ purpuric lesions develop involving the palms and soles. Arthritis and arthralgias are common features of Parvovirus B 19 infection in adults. The arthritis is usually symmetric and involves the peripheral joints. Parvovirus B19 infection is associated with decreased red cell production in normal hosts. In patients with underlying red blood cell disorders this infection can precipitate an aplastic crisis. Chronic anemia can develop following Parvovirus B19 infection in immunocompromised patients such as patients with Human Immunodeficiency Virus (HIV). Symptomatic or asymptomatic acute infection with Parvovirus B19 during pregnancy has been associated with fetal death.
Cytomegalovirus (CMV) is another common virus that can infect children and adults. Children often have mild or asymptomatic infection but adults can present with a mononucleosis-type illness. Pharyngitis, adenopathy, and splenomegaly are less common with CMV mono than with mononucleosis secondary to Epstein - Barr virus. Mild hepatitis is frequently seen with cytomegalovirus infection. The skin rash associated with CMV can be variable in appearance but is usually maculopapular. Primary CMV infection during pregnancy is often complicated by congenital CMV infection which can result in multiple organ dysfunction in the fetus and possible fetal death. Primary CMV infection in immunocompromised patients can result in significant invasive disease such as pneumonia, hepatitis, colitis, esophagitis, retinitis, encephalitis, and myelitis. CMV infection is common in children in daycare and seronegative parents can acquire CMV from exposure to body fluids of asymptomatic infected children. CMV can be sexually transmitted in adults.
Between 40 – 90 % of patients with acute HIV infection are symptomatic. The most common features of the Acute Retroviral Syndrome (ARS) are fever, pharyngitis, lymphadenopathy and rash. The rash is maculopapular and involves the face, trunk, and sometimes the extremities (including palms and soles). Mucosal ulcerations may occur in the mouth, esophagus or genital region. A history of unprotected sexual intercourse or sharing needles used for injection of recreational drugs would be an important clue. Recognition of the ARS is especially important as the high viral loads seen in acute infection can result in increased risk of transmission. The typical serologic tests for HIV may not be diagnostic with acute infection. Demonstration of viremia by polymerase chain reaction (PCR) in a patient with a consistent clinical syndrome supports the diagnosis of ARS.
Epstein - Barr virus is the most common etiology for infectious mononucleosis. Fever, pharyngitis, and lymphadenopathy characterize the acute illness. Rash occurs in about 5 % of patients and may be variable in nature (maculopapular, petechial, scarlatiniform, urticarial, or vesicular). Thrombocytopenia and a predominance of atypical lymphocytes are common hematological findings, but these findings can be seen with other acute viral infections such as CMV and HIV. Heterophile antibodies measured by the Monospot test are present in approximately 90 % of cases, so assay for EBV specific antibodies is rarely required for diagnosis. False positive Monospot test results are rare. Virus specific antibody testing may be useful in the small number of cases where the monospot test is negative.
Another herpesvirus, Human Herpesvirus 6 (HHV6), is the etiology of roseola or exanthem subitum. This is generally a mild disease in infants and children but it can cause a mononucleosis-like illness in adults. The rash associated with HHV6 is maculopapular in character, appears after resolution of fever, and spares the face. Acute hepatitis can be seen with primary HHV6 infection. Conversion from negative to positive or a four fold rise in titer for HHV6 IgG supports the diagnosis of primary infection. Assays for HHV 6 IgM may not be reliable. PCR for HHV 6 on plasma or serum may also be useful for diagnosis.
A variety of enterovirus infections can present with fever and rash. Most of the rashes are maculopapular but a few enteroviruses may produce a petechial or vesicular rash. Patients may have associated pharyngitis or diarrhea. Isolation of virus from throat or rectal swab is not diagnostic as patients can harbor enteroviruses and not be symptomatic. Enterovirus infections are seen predominantly in late summer and early fall but sporadic cases can be seen throughout the year. These viruses are the most common cause of aseptic meningitis.
Syphilis is caused by infection with the spirochete Treponema pallidum.
The second stage of syphilis
![]() usually presents 6 – 8 weeks after the primary
stage, but occasionally the chancre can still be present. Secondary syphilis is
characterized by fever, rash, and lymphadenopathy. The classic rash is a diffuse
maculopapular eruption that involves the palms and soles. Mucous patches may be
visible on mucous membranes. Moist gray papules called condylomata lata are
visible in the mouth or on the labia, anus or scrotum. These lesions are highly
infectious. Spirochetes can also be found within skin lesions. Patients with
secondary syphilis may have hepatosplenomegaly with mild elevation of
transaminases on laboratory exam. Headache and aseptic meningitis can be seen.
The Rapid Plasma Reagin (RPR) test should be positive at high titer with a
positive Fluorescent Treponemal Antibody absorption test (FTA-Abs).
Intramuscular injection of benzathine penicillin is still the treatment of
choice for primary and secondary syphilis. Untreated secondary syphilis can
result in late cardiac or neurological manifestations of disease. All patients
with syphilis should be tested for HIV. Sexual partners of patients diagnosed
with syphilis need to be evaluated and treated.
usually presents 6 – 8 weeks after the primary
stage, but occasionally the chancre can still be present. Secondary syphilis is
characterized by fever, rash, and lymphadenopathy. The classic rash is a diffuse
maculopapular eruption that involves the palms and soles. Mucous patches may be
visible on mucous membranes. Moist gray papules called condylomata lata are
visible in the mouth or on the labia, anus or scrotum. These lesions are highly
infectious. Spirochetes can also be found within skin lesions. Patients with
secondary syphilis may have hepatosplenomegaly with mild elevation of
transaminases on laboratory exam. Headache and aseptic meningitis can be seen.
The Rapid Plasma Reagin (RPR) test should be positive at high titer with a
positive Fluorescent Treponemal Antibody absorption test (FTA-Abs).
Intramuscular injection of benzathine penicillin is still the treatment of
choice for primary and secondary syphilis. Untreated secondary syphilis can
result in late cardiac or neurological manifestations of disease. All patients
with syphilis should be tested for HIV. Sexual partners of patients diagnosed
with syphilis need to be evaluated and treated.
| 28 year old HIV negative African American male with a history of multiple STDs. A maculopapular rash was present for 1-2 weeks. RPR was positive and rash resolved with treatment. | ||
|
|
 |
|
There are tick borne illnesses that can present with fever and rash. Rocky Mountain spotted fever (RMSF) has already been discussed, but it is important to point out that the rash of RMSF may be maculopapular early in the course of the illness. Tick borne illnesses peak in spring and summer. Ehrlichiosis refers to disease secondary to infection with rickettsia-like organisms that are transmitted by ticks. Human monocytotropic ehrlichiosis (HME) is caused by Ehrlichia chaffeensis and human granulocytotropic anaplasmosis (HGA) is caused by Anaplasma phagocytophilum. The tick vectors and the epidemiology are different for these diseases. HME cases have been reported predominantly from southeastern and south central United States, and HGA cases have been concentrated in the northeast, upper Midwest and parts of the west coast. The clinical features of the illnesses are very similar: fever, headache, malaise, myalgias. Rash occurs in approximately 30 % of adults and 60 % of children with HME, but rash is rare in HGA. The exanthem reported with ehrlichiosis is characterized as macular or maculopapular, and rarely involves the palms and soles. Gastrointestinal or respiratory symptoms may be present. Laboratory studies are significant for leukopenia, thrombocytopenia, and elevated transaminases. Rapid diagnosis of HGA can be made if morulae are identified on peripheral blood smear but the percentage of infected leukocytes is variable. Morulae are rarely seen in HME. No other rapid tests are routinely available; therefore empiric doxycycline should be started in patients with a history of tick exposure, travel to an area endemic for ehrlichiosis, and a consistent clinical syndrome. HME and HGA can be fatal if untreated. PCR and serology are available for diagnosis but results may not be available to aid in acute management. A third species, Ehrlichia ewingii, has been reported to cause a granulocytotropic picture of disease in immunocompromised hosts from Missouri, Tennessee, and Oklahoma.
Lyme disease, caused by the spirochete Borrelia burgdorferi, can present with flu-like symptoms and rash. The classic rash, erythema migrans (EM), develops 3 – 30 days after the tick bite. It is a rapidly enlarging erythematous macule often with central clearing resulting in a bull's eye appearance. The lesions are usually greater than 5 centimeters in diameter and occur on parts of the body where an attached tick may go unnoticed for 36 – 48 hours. Multiple EM lesions can be seen in a small percentage of patients. The history should suggest the potential for tick exposure in the northeast, upper Midwest or far west regions of the United States. Most cases occur between May and July, but transmission can be seen from early spring until late fall. As the vector is very small patients may not give a history of a tick bite. The diagnosis of early Lyme disease is usually a clinical diagnosis. Serology for B. burgdorferi may confirm the diagnosis in a patient with the appropriate clinical syndrome and exposure history. Doxycycline is the treatment of choice for early Lyme disease but other agents such as amoxicillin and cefuroxime may also be effective. Treatment of early Lyme disease is usually effective and prevents the development of late complications of Borrelia infection.
There are many other uncommon infections that present as fever and maculopapular rash. A discussion of all of these entities is beyond the scope of this chapter, but I would like to mention a few select syndromes. Dengue has already been mentioned in the discussion of petechial rash but Dengue can present with a more generalized erythematous macular rash. Clearly an appropriate travel history would be an important clue. Typhoid fever is associated with centrally-distributed, erythematous macules or papules. The organism, Salmonella typhi, can be cultured from skin lesions in about 50 % of cases but blood cultures are usually positive. Typhoid fever may be in the differential of fever and rash in the returned traveler. Typhus can present with fever and maculopapular rash. Louse-borne Typhus is caused by infection with Rickettsia prowazekii. This disease has been associated with epidemics throughout the world and is endemic in many locations worldwide. The rash involves the trunk and extremities, but spares the face, palms, and soles. The clinical presentation may also include conjunctival injection and headache. Murine Typhus is caused by infection with Rickettsia typhi and is transmitted by fleas. The disease can be seen worldwide but in the United States most cases have been seen in southern Texas and California. Patients present with fever, headache, myalgias, and a maculopapular rash that involves the trunk and extremities including the palms and soles. Serology is the main means of diagnosis for both of these diseases but results generally are not available for acute management and early diagnosis is based on clinical suspicion. Doxycycline is the treatment of choice for Typhus.
Leptospirosis, psittacosis, and rate-bite fever are uncommon causes of fever and rash syndrome seen in patients with specific exposure histories. Leptospira infection is acquired from direct or indirect contact with urine or tissue from infected animals. The organisms enter via compromised skin, mucous membranes or inhalation. Patients present with fever, headache, myalgias, nausea and vomiting. Conjunctival suffusion is common but the pretibial maculopapular rash is rare. Lab studies reveal thrombocytopenia, and an elevated BUN and bilirubin. The illness can be biphasic with the second phase complicated by renal and hepatic failure. Most diagnoses are made by serology. Treatment is based on the severity of the disease but doxycycline, penicillin, and ceftriaxone are all effective. Chlamydia psittaci infection is usually associated with contact with birds. The presentation can be variable but fever, headache and cough are common. The classic skin manifestation, Horder's Spots, are pink maculopapular lesions that occur on the trunk. A wide variety of other rashes have been described with psittacosis. Serology can be diagnostic and tetracycline is the drug of choice. Rate Bite Fever caused by Streptobacillus moniliformis can be acquired from a rate bite or by ingestion of contaminated food. Patients have fever, severe polyarthritis and rash. The rash can be maculopapular, vesicular, pustular or petechia; and is concentrated on the hands, feet, palms and soles. Blood cultures are usually positive and the organism is susceptible to penicillin.
VESICLES/BULLAE (Table 7)
Varicella, caused by the herpesvirus Varicella Zoster Virus (VZV), is a common
cause of fever and generalized vesicular rash
![]() (a). The epidemiology of this disease
may change in the near future with increasing use of the Varicella vaccine.
Infection occurs as a result of exposure to infectious respiratory secretions or
material from a Varicella or Zoster skin lesion. An individual is infectious
prior to development of the rash therefore patients may be unaware of the
exposure. The peak incidence is in the spring. Patients present with fever and
malaise followed by rash, which is characterized as vesicles on an erythematous
base. The lesions crust and gradually heal. Lesions in different stages of
evolution are seen on exam. Complications include bacterial superinfection,
pneumonia
(a). The epidemiology of this disease
may change in the near future with increasing use of the Varicella vaccine.
Infection occurs as a result of exposure to infectious respiratory secretions or
material from a Varicella or Zoster skin lesion. An individual is infectious
prior to development of the rash therefore patients may be unaware of the
exposure. The peak incidence is in the spring. Patients present with fever and
malaise followed by rash, which is characterized as vesicles on an erythematous
base. The lesions crust and gradually heal. Lesions in different stages of
evolution are seen on exam. Complications include bacterial superinfection,
pneumonia
![]() (b), and encephalitis. The latter are more likely to develop in adults.
Reye's syndrome may be a complication in both children and adults. If
hospitalized, patients with suspected or proven Varicella should be placed in
strict isolation. Virus can be cultured from skin lesions but the results may
take days and culture may not be available outside of tertiary care
institutions. A rapid diagnosis can be made by staining cells obtained from the
base of a lesion with a monoclonal antibody to specific VZV proteins tagged with
a fluorescent marker. This Direct Fluorescent Antibody (DFA) testing may not be
routinely available but can provide a specific diagnosis within hours. Local
recurrence of VZV, Zoster, can occur with dissemination especially in
immunocompromised hosts. Primary infection with Herpes Simplex virus 1 or 2,
either in the oral or genital regions, can be associated with fever and a
localized vesicular rash. Disseminated herpes simplex virus (HSV) infection also
presents with fever and diffuse vesicular rash and occurs more frequently in
immunocompromised patients or patients with severe eczema. Visceral involvement,
especially hepatitis, is common. The mortality from disseminated HSV is higher
than that from disseminated Zoster. The skin lesions are indistinguishable but
the DFA can rapidly differentiate HSV and VZV. Acyclovir is effective for both
HSV and VZV but the dosing is different for the two viruses. Smallpox, Variola,
causes fever and a disseminated vesicular rash. In contrast to the rash seen
with Varicella, in smallpox all of the skin lesions are at the same stage. The
rash of smallpox is concentrated on the face and extremities including the palms
and soles, where as the rash of Varicella is more concentrated on the trunk. The
CDC website includes tools to assist practitioners in the assessment of patients
with disseminated vesicular rash. State and local health departments should be
notified immediately in the case of suspected smallpox.
(b), and encephalitis. The latter are more likely to develop in adults.
Reye's syndrome may be a complication in both children and adults. If
hospitalized, patients with suspected or proven Varicella should be placed in
strict isolation. Virus can be cultured from skin lesions but the results may
take days and culture may not be available outside of tertiary care
institutions. A rapid diagnosis can be made by staining cells obtained from the
base of a lesion with a monoclonal antibody to specific VZV proteins tagged with
a fluorescent marker. This Direct Fluorescent Antibody (DFA) testing may not be
routinely available but can provide a specific diagnosis within hours. Local
recurrence of VZV, Zoster, can occur with dissemination especially in
immunocompromised hosts. Primary infection with Herpes Simplex virus 1 or 2,
either in the oral or genital regions, can be associated with fever and a
localized vesicular rash. Disseminated herpes simplex virus (HSV) infection also
presents with fever and diffuse vesicular rash and occurs more frequently in
immunocompromised patients or patients with severe eczema. Visceral involvement,
especially hepatitis, is common. The mortality from disseminated HSV is higher
than that from disseminated Zoster. The skin lesions are indistinguishable but
the DFA can rapidly differentiate HSV and VZV. Acyclovir is effective for both
HSV and VZV but the dosing is different for the two viruses. Smallpox, Variola,
causes fever and a disseminated vesicular rash. In contrast to the rash seen
with Varicella, in smallpox all of the skin lesions are at the same stage. The
rash of smallpox is concentrated on the face and extremities including the palms
and soles, where as the rash of Varicella is more concentrated on the trunk. The
CDC website includes tools to assist practitioners in the assessment of patients
with disseminated vesicular rash. State and local health departments should be
notified immediately in the case of suspected smallpox.
| (a) Vesicles (Green arrows)- Fluid-filled, elevated lesion less than 1 cm in diameter; Bulla (Red arrows)- Fluid filled, elevated lesions > 1 cm in diameter | (a) Pus-filled vesicle | (b) 29 year old developed shortness of breath following exposure to a child with chicken pox. Dermatologic findings were consistent with acute Varicella zoster and the patient reported no previous history of clinical infection. |
|
|
|
 |
Disseminated infection with Vibrio vulnificus can result in bullous skin lesions. Persons usually acquire the organism through contact of non-intact skin with salt water or through ingestion of raw seafood. Patients with chronic liver disease, especially cirrhosis, are at increased risk of developing sepsis with this organism. The cellulitis with shock is similar in presentation to group A beta hemolytic streptococcus infection. The history of exposure to salt water or raw seafood should be a clue. Patients can have bullae at the site of the cellulitis or scattered bullae with dissemination of the infection. The lesions heal with eschar. Cultures from skin lesions and blood are usually positive. Tetracycline with or without cefotaxime is the recommended treatment.
Localized skin infection with Aeromonas sps can result in a vesiculobullous eruption. This organism has been associated with fresh water exposure to non-intact skin, and the medicinal use of leeches. Ciprofloxacin, ceftazidime or carbapenems are effective treatments.
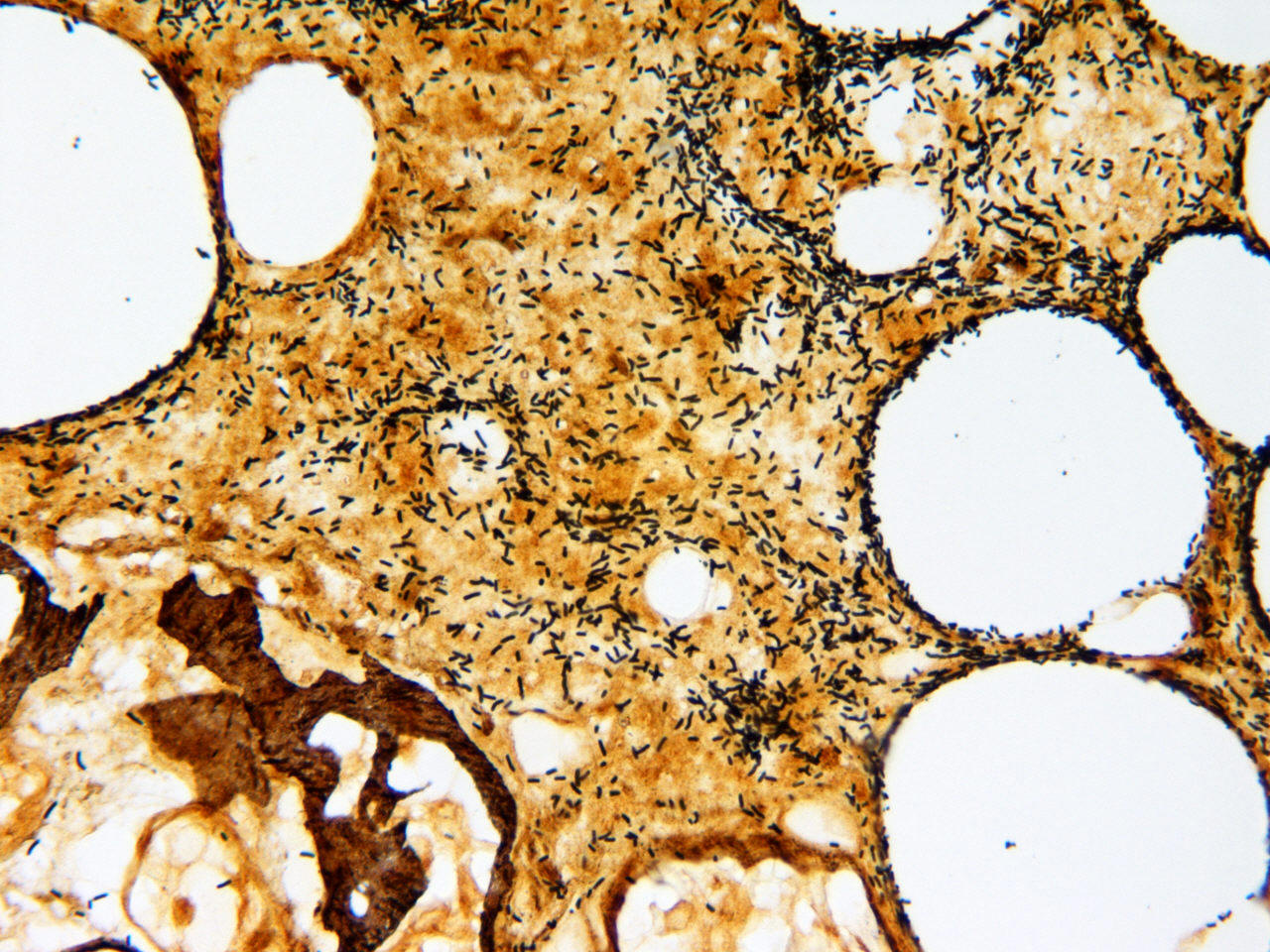
Pseudomonas aeruginosa septicemia, especially in neutropenic hosts, can
present with scattered skin lesions. The classic skin lesion is ecthyma
gangrenosum
![]() , which is described as an erythematous, indurated lesion with
bullous formation followed by ulceration. Blood cultures are commonly positive
in patients with ecthyma gangrenosum. In neutropenic patients empiric antibiotic
therapy usually includes an anti-pseudomonal penicillin or cephalosporin and an
aminoglycoside. Pseudomonas has also been associated with generalized
vesiculopustular lesions associated with hot tub exposure.
, which is described as an erythematous, indurated lesion with
bullous formation followed by ulceration. Blood cultures are commonly positive
in patients with ecthyma gangrenosum. In neutropenic patients empiric antibiotic
therapy usually includes an anti-pseudomonal penicillin or cephalosporin and an
aminoglycoside. Pseudomonas has also been associated with generalized
vesiculopustular lesions associated with hot tub exposure.
| 60 year old malnourished female burn patient with Pseudomonas bacteremia and biopsy confirmed ecthyma gangrenosum. The sliver stain of the biopsy showed fat necrosis and numerous bacilli (Pseudomonas). | ||
|
|
 |
 |
Disseminated Neisseria gonorrhoeae presents with fever, arthritis, tenosynovitis, and a pustular rash that is found predominantly on the extremities. Blood cultures are often positive but synovial fluid and skin biopsies are usually sterile. Neisseria gonorrhoeae can be recovered from a mucosal site in approximately 80 % of patients with disseminated gonococcal infection (DGI). Patients should be treated with ceftriaxone initially but can be switched to oral cefixime or a quinolone once they demonstrate clinical improvement.
Staphylococcal scalded skin syndrome has been discussed in this chapter. Although patients have diffuse erythema initially there is secondary bulla formation. Necrotizing soft tissue infections with group A streptococci or Clostridium sps can also demonstrate bullae formation. Enteroviral infections can be associated with vesicular rash. Erysipelothrix rhusiopathiae is a gram positive rod that is associated with skin infection following exposure to a variety of animal tissue. Individuals at greatest risk include fish handlers, butchers, and veterinarians. Vesiculation may occur at the site of cellulitis but systemic symptoms such as fever are rare with localized disease. Disseminated disease is unusual.
As mentioned previously enteroviral infections can present with variable skin manifestations. Many enteroviruses have been associated with Hand-Foot-and-Mouth disease (HFM). The disease is seen most commonly in children. Patients present with fever and sore throat or mouth. Vesicles can be seen in the oral cavity, usually on the buccal mucosa or tongue. The exanthema is seen predominately on the hands and feet but may occur at other sites. The skin lesions are papular to vesicular and have a rim of surrounding erythema similar to the lesions of HSV or VZV.
Lesions of erythema multiforme have central erythema surrounded by normal-appearing skin that in turn is surrounded by another ring of erythema. The central area often vesiculates. These lesions are usually symmetric in their distribution and involve the palms and soles. Mucosal involvement is often present. When there is extensive mucosal involvement with conjunctivitis and stomatitis the term Stevens - Johnson syndrome is applied. Drugs are the most common etiology for erythema multiforme, but it is associated with a variety of infectious agents including mycoplasma, HSV and other viruse.
Table 7. Infections Associated with Vesicobullous/Pustular Lesions
Varicella Disseminated Zoster Disseminated HSV Vibrio vulnificus Pseudomonas aeruginosa Aeromonas sps Enteroviruses Smallpox Disseminated Neisseria gonorrhoeae Erysipelothrix rhusiopathiae Note: bullae can be seen with SSSS and with necrotizing soft tissue infections
ESCHAR
In several infections the primary lesion may be a papule, which forms a vesicle
that leads to ulcer formation and eschar
![]() . The primary papule may go unnoticed
and the eschar is the skin manifestation that is seen at the time of
presentation with fever and localized adenopathy (Table 8). Some of these
infections are of particular interest because of their potential role in
bioterrorism. Tularemia is caused by infection with Francisella tularensis.
Humans can acquire the infection by handling infected rodents; tick, fly, or
mosquito bite; inhalation of infected material, or occasionally by animal bite.
An eschar develops at the site of skin inoculation within 3 – 10 days, and there
are associated tender regional lymph nodes, fever, headache, and malaise.
Diagnosis is usually by serology. Tularemia can be treated with a variety of
different antimicrobials including streptomycin, gentamicin, doxycycline, and
ciprofloxacin.
. The primary papule may go unnoticed
and the eschar is the skin manifestation that is seen at the time of
presentation with fever and localized adenopathy (Table 8). Some of these
infections are of particular interest because of their potential role in
bioterrorism. Tularemia is caused by infection with Francisella tularensis.
Humans can acquire the infection by handling infected rodents; tick, fly, or
mosquito bite; inhalation of infected material, or occasionally by animal bite.
An eschar develops at the site of skin inoculation within 3 – 10 days, and there
are associated tender regional lymph nodes, fever, headache, and malaise.
Diagnosis is usually by serology. Tularemia can be treated with a variety of
different antimicrobials including streptomycin, gentamicin, doxycycline, and
ciprofloxacin.
Table 8. Fever, Eschar and Adenopathy Eschar :hard crust or scab
Tularemia
Anthrax
Rickettsia sps
Plague
Anthrax, caused by Bacillus anthracis, has received a great deal of attention because of its use as a bioterrorism agent. Human infection with anthrax has been associated with infection in cattle or other herbivores such as goats, horses, and sheep. A variety of animal products can be contaminated with the organism and can facilitate transmission of the infection: hides, wool, hair, meat, bones, and bone meal. Anthrax spores can survive for prolonged periods of time in the environment depending on environmental conditions. Spores can be inoculated into skin, ingested, or inhaled. The skin lesion develops 1 – 12 days after exposure and initially is characterized as a pruritic papule. The papule develops a vesicular center and eventual eschar formation. There is often surrounding non-pitting edema, associated tender lymphadenopathy, and satellite lesions. Systemic symptoms of fever, headache and malaise may be present. The skin lesions are usually not painful and microscopic examination of the skin lesion fails to reveal inflammatory cells. The organism can be cultured from specimens of exudates, skin, or blood obtained prior to initiation of antibiotics. For disease not associated with bioterrorism penicillin is the drug of choice but ciprofloxacin is recommended for empiric treatment in cases where bioterrorism is suspected.
Yersinia pestis, the organism that causes plague, has also received a great deal of interest as a potential bioterrorism agent. Infection can occur via the inhalation route but the most common means of transmission is through the bite of a flea from an infected rodent. Illness characterized by fever, headache, and tender enlarged lymph nodes (buboes) develops within 2 – 7 days of the bite. Even with careful exam the primary skin lesion can only be found in about 25 % of cases. Microscopic examination of skin lesions demonstrates polymorphonuclear cells and gram negative bacilli. Material for culture can be obtained from blood, buboes, or skin lesions. Serology is available but may not be useful for acute management. The aminoglycosides streptomycin and gentamicin are the drugs of choice but doxycycline and ciprofloxacin may also be effective. Public health authorities need to be notified of any cases of suspected bioterrorism.
Rickettsialpox, caused by Rickettsia akari and transmitted by the mouse mite, occurs worldwide. A papule forms at the site of the bite and eventually transforms into an eschar. There is fever, headache and associated tender lymphadenopathy. A more disseminated rash develops and goes through a similar series of stages: papule→vesicle→eschar. The palms and soles are spared. Diagnosis is by serology and treatment is doxycycline. There are a number of Rickettsia sps that are transmitted by ticks and present with a picture of fever, headache, inoculation eschar and regional lymphadenopathy. Each species has a specific geographic distribution and cases identified in the United States are seen in returning travelers. (See discussion of fever in the returned traveler). Doxycycline is the treatment of choice for all of these rickettsia infections.
NODULES
Most of the illnesses associated with fever and nodular skin lesions
![]() are
confined to patients who are immunocompromised (Table 9). The most common groups
include patients with hematological malignancies, patients status post solid
organ or bone marrow transplantation, and patients with Acquired
Immunodeficiency Syndrome (AIDS). (Please see chapters on fever in organ
transplant recipients, patients with neutropenia, and patients with HIV
infection). The most common etiologies are fungi and atypical mycobacteria. In
patients with leukemia Candida is the most common isolate. The skin
nodules are well circumscribed, firm and erythematous often with a pale center.
Similar skin lesions can be seen with a variety of other fungi: Sporothrix,
Aspergillus, Mucor, Cryptococcus, Coccidioides, Histoplasma, and
Fusarium. Travel history to the Ohio River valley or
to the southwestern United States may be useful clue for Histoplasma and
Coccidioides respectively. Atypical mycobacteria can cause disseminated
nodular lesions in immunocompromised hosts. These lesions may be violaceous in
color and can ulcerate and drain. Skin biopsy is the best means of diagnosis.
Tissue should be sent for smear and culture for AFB and fungus. Nocardia can
also cause nodular skin lesions in immunocompromised patients. Especially in
patients with AIDS, Bartonella henselae or B. quintana infection
can cause bacillary angiomatosis, a systemic illness characterized by fever and
nodular skin lesions. The skin lesions often have a vascular appearance and may
be confused with the lesions of Kaposi Sarcoma. Blood cultures may be positive
but skin biopsy should be diagnostic. Serology or PCR for Bartonella
species can also be performed. A history of cat exposure should be a clue for
bacillary angiomatosis.
are
confined to patients who are immunocompromised (Table 9). The most common groups
include patients with hematological malignancies, patients status post solid
organ or bone marrow transplantation, and patients with Acquired
Immunodeficiency Syndrome (AIDS). (Please see chapters on fever in organ
transplant recipients, patients with neutropenia, and patients with HIV
infection). The most common etiologies are fungi and atypical mycobacteria. In
patients with leukemia Candida is the most common isolate. The skin
nodules are well circumscribed, firm and erythematous often with a pale center.
Similar skin lesions can be seen with a variety of other fungi: Sporothrix,
Aspergillus, Mucor, Cryptococcus, Coccidioides, Histoplasma, and
Fusarium. Travel history to the Ohio River valley or
to the southwestern United States may be useful clue for Histoplasma and
Coccidioides respectively. Atypical mycobacteria can cause disseminated
nodular lesions in immunocompromised hosts. These lesions may be violaceous in
color and can ulcerate and drain. Skin biopsy is the best means of diagnosis.
Tissue should be sent for smear and culture for AFB and fungus. Nocardia can
also cause nodular skin lesions in immunocompromised patients. Especially in
patients with AIDS, Bartonella henselae or B. quintana infection
can cause bacillary angiomatosis, a systemic illness characterized by fever and
nodular skin lesions. The skin lesions often have a vascular appearance and may
be confused with the lesions of Kaposi Sarcoma. Blood cultures may be positive
but skin biopsy should be diagnostic. Serology or PCR for Bartonella
species can also be performed. A history of cat exposure should be a clue for
bacillary angiomatosis.
Erythema nodosum is characterized by tender erythematous nodules usually confined to the lower extremities. These skin lesions are seen in association with a wide variety of non-infectious, inflammatory illnesses and are felt to be immune mediated. Infectious agents such as Yersinia, Chlamydia, fungi, and Mycobacterium tuberculosis can trigger erythema nodosum. Sweet's syndrome, or febrile neutrophilic dermatosis, presents with fever and nodular skin lesions that ulcerate. The etiology is unclear but it occurs predominately in individuals with hematological malignancies or other underlying disease. Biopsy of the skin lesion reveals a characteristic neutrophilic infiltrate.
Table 9. Infections Associated with Nodules Nodule: rounded, elevated lesion > 1 cm in diameter
Candida Mycobacterium haemophilum Mucor Mycobacterium chelonae Fusarium Mycobacterium fortuitum Aspergillus Cryptococcus Sporothrix Histoplasma Coccidioides
URTICARIA
Urticaria and fever are rarely associated with active infection (Table 10). It is estimated that up to 25 % of patients with acute Hepatitis B will develop a serum-sickness-like reaction that includes a rash that can be urticarial in nature. Certain enteroviruses are associated with urticarial eruptions. A variety of parasitic infections can be associated with urticarial rash: acute schistosomiasis, strongyloidiasis, filarial infection such as Loa loa, and trichinosis.
Table 10. Urticaria
- Acute Hepatitis B
- Schistosomiasis
- Strongyloidiasis
- Trichinosis
- Filarial infections