
Sepsis - Management
SOURCE CONTROL
While antimicrobial therapy can be life saving, some patients cannot be successfully treated without removing or draining the site of infection. When patients have septic shock due to an infected catheter, patients are far more likely to have a successful outcome if the catheter is promptly removed. Similarly, if the source of sepsis, severe sepsis, or septic shock is an infected foreign body such as a joint prosthesis, a pacemaker, or an Omaya shunt, that device must be removed to optimize outcome. Foreign bodies such as biliary stints, urinary stints, Foley catheters, chest tubes, or ventriculostomies must usually be removed to optimize outcome. There are, however, some specific syndromes and specific pathogens that can be treated medically if there is an urgent need to do so, without removing the foreign body.
Collections of purulent fluid must be drained in most situations. Urosepsis associated with an obstructed ureter, a pneumonia with an associated empyema, a liver abscess, or a renal abscess are examples of collections that must be drained to optimize outcome. How that drainage is accomplished depends on the location, the infection, and the patient. In some situations needle drainage is adequate; in other situations more extensive surgical drainage is required. In some situations, such as brain abscesses and liver abscesses, medical therapy alone can be successful, but such an approach requires judgment, careful evaluation of the literature, with focus on how ill the patient is and what the risks and benefits of the technical options are.
EMPIRIC ANTIMICROBIAL THERAPY
The urgency of empiric therapy depends on the severity of the clinical syndrome and the vulnerability of the host. For some patients, there is no urgency to start therapy until the offending pathogen is identified. For others with severe sepsis or septic shock, empiric therapy is life saving, i.e. antimicrobial therapy must be started before the specific pathogen or, in some cases, before the site of infection, is identified.
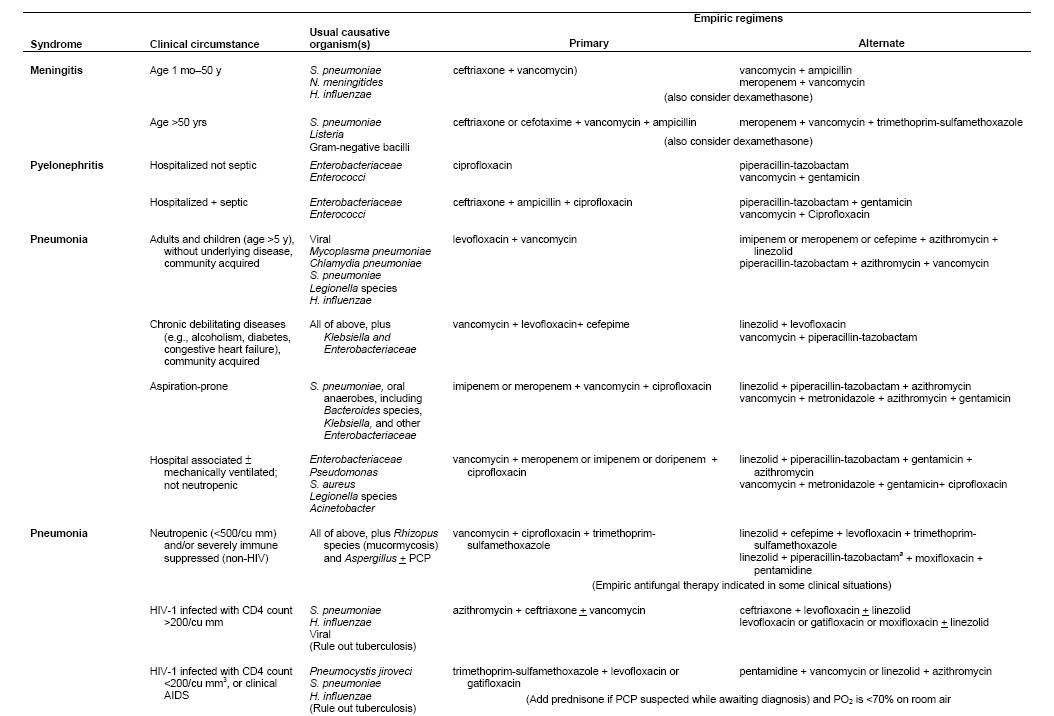
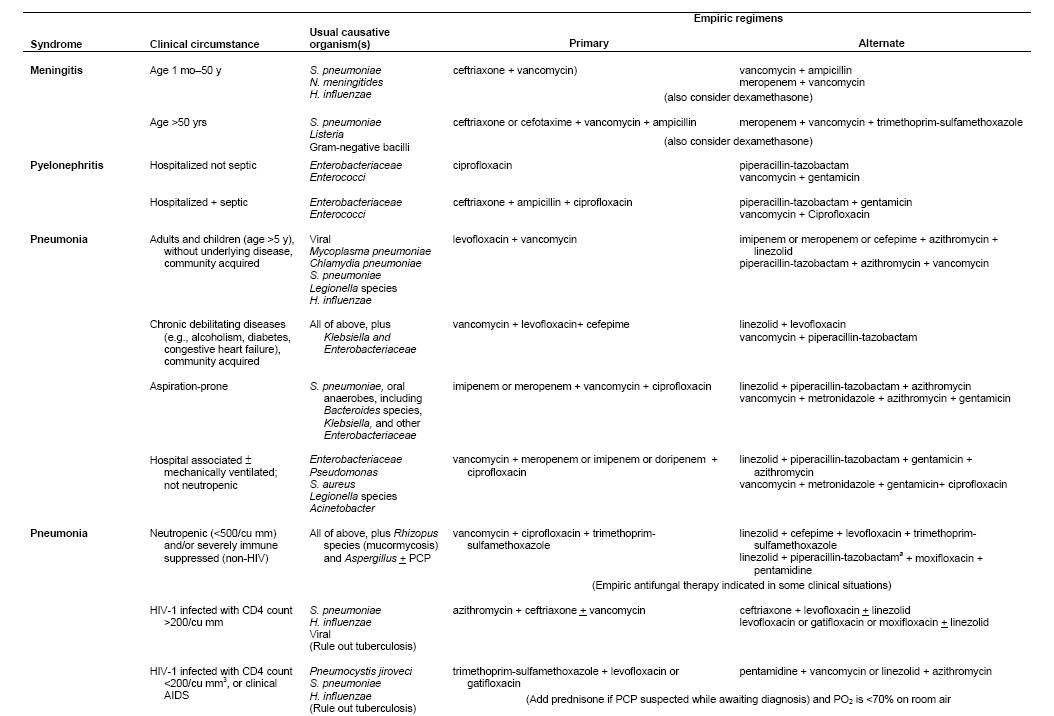
Table 4 provides some potential empiric regimens for the therapy of septic shock. Many possible regimens could be used with similar results. The choice in each situation depends on the pathogens likely to cause a specific infectious syndrome, knowledge of organisms the host has been colonized with, consideration of what antibiotics the patient has recently been exposed to, local epidemiologic trends in pathogens and resistance patterns, and patient ability to tolerate specific agents.
When developing regimens, particular attention should be given to MRSA and Candida, in addition to pathogens such as Acinetobacter or Pseudomonas that may be especially prevalent in a given setting. For seriously ill patients, MRSA has become especially common in many areas when skin, soft tissue, catheter, or pulmonary infections are involved, or when patients present with sepsis of unknown source. Thus, antibiotic coverage for MRSA should be universally considered, i.e. there should usually be a clearly articulated rationale for not including such coverage.
Candida is the fourth most common pathogen causing blood stream infections in intensive care units. Moreover, candidemia is increasingly common among patients with central venous catheters, arterial catheters, neutropenia, and complicated gastrointestinal surgical procedures. Since time to initiation of therapy for Candida correlates with outcome, consideration of an antifungal agent should be part of the initial management algorithm. For patients with severe sepsis or septic shock, the initiation of appropriate therapy is urgent. Several observational data bases have demonstrated that outcome become progressively less favorable the longer the interval until appropriate therapy is started. Thus, initial regimens need to be broad in order to be certain that the causative agent is treated. The initial regimen can subsequently be narrowed when the causative agent is definitively identified. The initial agent must be infused into the patient promptly, and not merely ordered in the computer: the system involved in transferring a cognitive plan to administer antibiotics to the successful infusion into the patient involves many steps that require the medical, nursing, pharmacy and information technology programs to work cohesively. In most hospitals, a substantial number of patients do not receive their antibiotics within 30-60 minutes of an order being written. For septic shock in particular, clinicians must work with nursing and pharmacy to assure that the patient has enough ports for infusion, that infusion times of individual drugs are considered in their selection and prioritization. Clinicians must recognize that blood cultures will be negative > 50% of patients with septic shock. Thus, once a clinical diagnosis of severe sepsis or septic shock has been established, patients should receive a full course of therapy (usually 7-10 days) unless another cause of the syndrome has been conclusively identified.
Table 4: Examples of Some Empiric Regimens for Several Presentations of Sepsis (Note that all examples should be interpreted in the context of individual patient factors and pathogen susceptibility patterns at different hospitals).
SPECIFIC ANTIMICROBIAL THERAPY
Once the causative pathogen has been conclusively identified and antibiotic susceptibility results have been obtained, the broad empiric regimen can usually be narrowed. Clinicians must recognize, however, that certain infectious syndromes may be polymicrobial. Finding a single organism in the bloodstream does not invariably indicate that only a single organism is involved. For instance, in a patient with a colonic perforation, finding E. coli in 4 blood cultures is useful information, but the likelihood is that many other aerobic and anaerobic organisms care also pathologically important in causing the septic syndrome. Thus, judgment is required in determining whether to narrow the spectrum of antibiotic therapy. In contrast, if Streptococcus pneumoniae is isolated from the bloodstream in a patient with sepsis and pneumonia, it is extremely likely this is the sole pathogen, and antibiotic therapy can be significantly narrowed.
There has been considerable debate in the past about the use of bactericidal antibiotics versus bacteristatic drugs. Except for endocarditis, there has been no evidence that bactericidal drugs are more effective, i.e. that their use produces improved patient outcome. Many clinicians prefer bactericidal drugs for neutropenic patients or for severely ill patients. However, there is no clinical evidence support this preference. There has also been debate regarding the desirability of combination therapy versus combination therapy for treatment of a specific pathogen. Combination therapy is a logical strategy in terms of assuring that the breadth of coverage include all likely pathogens when patients are severely ill, and there is no margin for error. However, for treating specific pathogens, there are few examples in which combination therapy is superior to monotherapy when modern, potent agents are used.
The optimal duration of antibiotic therapy has not been studied for most types of sepsis, severe sepsis, and septic shock. The duration of therapy will be determined by the rapidity of host improvement, host immunologic status, presence of undrained purulence or unremoved foreign bodies. While 7-10 days in non neutropenic patients with no undrained focus is often recommended, there is little data on which to base this recommendation on. Moreover, there are situations where shorter courses are clearly effective. The optimal drugs for specific microorganisms isolated in septic patients can be found in other chapters in this book.
ADJUNCTIVE THERAPIES FOR SEPSIS AND SEPTIC SHOCK
The four essential components of early therapy for patients with sepsis or septic shock are: source control, prompt administration of empiric antibiotics that take into account the most likely pathogen and anti-microbial sensitivity, fluid and vasopressor administration to maintain organ perfusion and source control (i.e., drainage of abscess, removal of infected hardware etc). Several adjunctive therapies are also commonly used although the evidence supporting their efficacy is less convincing.
Fluid Resuscitation and Vasopressors
Severe sepsis or septic shock requires fluid resuscitation in order to maintain perfusion of vital organs. The usual treatment approach for severe sepsis or septic shock in adults is to initiate fluid support using either boluses crystalloid (1000 ml of normal saline or Ringer’s lactate) or colloid (500 ml of 5% albumin) given over 15 to 30 minutes with a goal to maintain a mean arterial pressure of ≥ 65 mmHg or a systolic blood pressure of ≥ 90 mmHg. Hydroxyethyl starch is not recommended since it is associated with higher rates of renal failure. Fluid resuscitation should be guided by hemodynamic monitoring (preferably with an arterial line and a central venous catheter), and evidence of end organ perfusion (e.g., urine output >0.5ml·kg-1·hr-1, lactate<4mmol/L and maintenance of mental status). If resuscitation goals are not being promptly achieved after several liters of fluid or if clinical evidence of pulmonary edema develops then vasopressor therapy should be administered via a central line. Norepinephrine has emerged as the standard vasopressor agent for septic shock although other vasopressors are used including dopamine less commonly epinephrine. There is a theoretical advantage to treating septic shock patients with low dose vasopressin; however, in a large prospective trial the use of vasopressin in conjunction with norepinephrine did not confer a survival benefit. Nonetheless, adjunctive vasopressin therapy should be considered as a rescue maneuver in patients with septic shock who are not responding to either norepinephrine or dopamine alone.
Glucocorticoids
The use of glucocorticoids in sepsis is controversial. Meta-analysis has shown that low doses (hydrocortisone 200 to 300mg daily for 5 to 7 days) confer a mortality benefit in severely septic patients. A recent trial of septic shock patients with a relatively low mortality rate (control group mortality 36%) showed that steroid therapy reduced the duration of hypotension, but had no mortality benefit. In light of these data, a reasonable approach is to consider low dose glucocorticoid therapy in severely ill septic shock patients who are not improving (i.e., vasopressor refractory shock) with standard treatment. Once steroid therapy is initiated, there should be a low threshold for suspecting occult secondary infections as bacteremic patients on steroids will not consistently mount a fever response.
Intensive Insulin Therapy
Intensive insulin therapy (serum glucose maintained between 80-110 mg/dl) has been proposed as an adjunctive therapy for sepsis based upon one trial--performed in critically ill postoperative surgical patients—that showed a survival benefit. In two subsequent trials of intensive insulin therapy, including one study which specifically enrolled severe septic patients, there was no mortality benefit due to intensive insulin therapy. Importantly, episodic severe hypoglycemia (< 40mg/dl) occurred at an unacceptably high rate. In light of the absence of reproducible benefit and the potential harm, intensive insulin therapy is not recommended for septic patients.
Early Goal Directed Therapy
Early goal directed therapy (EGDT) in sepsis is defined as prompt fluid resuscitation targeting optimal central venous pressure, mean arterial pressure and central venous oxygenation saturation (ScvO2). While the benefit of treating septic patients in a timely fashion is self-evident, the evidence that measuring ScvO2 is beneficial is less than compelling. In the only prospective trial of EGDT patients in the treatment arm differed from the controls in one aspect: a catheter capable of measuring ScvO2 was used to guide red blood cells transfusions or dobutamine administration. This one positive trial contrasted with the only other prospective trial evaluating titrating therapy to ScvO2 (albeit in critically ill patients) which showed no benefit. There have been no further trials testing EGDT (specifically ScvO2-guided therapy) as a stand-alone treatment. Analysis of these trials and other data cast doubt as to the contribution of ScvO2 monitoring to patient outcome. Thus, at this time such ScvO2 catheters should not be considered necessary for achieving optimal outcome despite their inclusion in well publicized guidelines and bundles.
Drotrecogin alfa
Activated protein C (drotrecogin alfa) is a component of the coagulation cascade and functions as an inhibitor of factors Va and VIIIa thereby promoting fibrinolysis. In addition, drotrecogin alfa has anti-inflammatory properties and is capable of inhibiting proinflammatory cytokine production. Low plasma levels of protein C occur in septic patients. Based upon the results of a single randomized controlled trial, this adjunctive therapy was approved for patients in septic shock who had a severity of illness score (APACHE II) greater than 25 within 24 hours of the onset of shock. Drotrecogin alfa is administered as a 96 hour infusion. Two subsequent randomized controlled trials, one pediatric study and another in adults septic patients with a low likelihood of death (APACHE II < 25), were both stopped early on the grounds of futility. An increased risk of serious bleeding including intracerebral hemorrhage, however, has been observed in all trials of drotrecogin alfa. Pending the results of an ongoing confirmatory trial of (PROWESS-SHOCK), drotrecogin alfa has the potential to cause serious bleeding and should be viewed as an optional therapy in patients with sepsis and a high likelihood of death.
CONCLUSION
Sepsis is a major cause of morbidity and mortality in the United States. Recognition of sepsis, severe sepsis or impending septic shock in the emergency department and in hospitalized patients remains a challenge that requires clinical judgement. Management principles for patients with distributive shock focus on an expeditious response involving source control, antimicrobial therapy, fluids, vasopressors and adjunctive therapies. Health care providers and medical facilities have an obligation to develop a systems based approach to assure that therapy is prompt, coordinated, and comprehensive in order to provide optimal patient outcome.