
Necrotizing Soft Tissue Infections - Definition and Causes
Necrotizing soft tissue infections are infrequent but highly lethal infections. It is estimated that there are between 500-1,500 new cases of necrotizing soft tissue infections per year in the US and a recent epidemiologic population-based study estimated the incidence of necrotizing soft tissue infections to be approximately 0.04/1,000 person-years with information derived from an insurance administrative database from various states in the United States. It is unclear if the incidence of this disease is increasing. However, its aggressive course, poor prognosis, and media-mediated awareness have certainly raised interest in the medical and general community. It is associated with devastating consequences including high mortality, disfigurement, disability, long-term rehabilitation and significant costs and resource utilization. Necrotizing soft tissue infections occur frequently enough that most primary care physicians, surgeons, and infectious disease specialists will see one or more during a professional career, but are infrequent enough that few will have significant experience and confidence in dealing with them.
DEFINITION AND NOMENCLATURE
Since the first description of necrotizing soft tissue infections by Jones, multiple terms have been used to define different kinds of necrotizing infections of the soft tissues. The terms used have been based on anatomic location of infection, soft tissue compartment involved, microbiologic and clinical features. Table 1 lists the different terms used to refer to necrotizing soft tissue infections. These terms have been used in an attempt to define “different” entities or to classify necrotizing soft tissue infections according to the above variables. But the reality is that the use of all these different definitions only leads to confusion and lacks any clinical or academic purpose.
Necrotizing soft tissue infections are defined by the presence of a spreading infection in any of the layers of the soft tissues (skin, subcutaneous tissue, superficial fascia, deep fascia, or muscles) which is associated with the presence of necrosis of the layer/s involved and hence requires surgical debridement. All necrotizing soft tissue infections fulfill this definition and have common features in their clinical presentation and diagnosis, and most importantly, all of these infections by definition require surgical debridement. It is because of this that labeling or classifying them with different terms does not serve a useful purpose and may in fact complicate management by delaying diagnosis and/or delaying surgical debridement. The true discriminative information that is essential for the management of soft tissue infections is the presence or absence of a necrotizing component and this should be the focus during the initial assessment of patients with soft tissue infections. As we will describe in the coming sections, narrowing the type of necrotizing soft tissue infections to Group A β-hemolytic Streptococcus (GAS) or clostridial infection may be useful in better defining prognosis and in identifying patients that may benefit from additional treatment options. However, the general presentation, diagnosis, and management follow the same principles and we encourage the use of the unifying term necrotizing soft tissue infections when referring to all these entities.
Table 1. Common Terms Used to Refer to Specific Types of Necrotizing Soft Tissue Infections
Different nomenclature
Hospital gangrene
Hemolytic streptococcal gangrene
Phagedena
Meleney’s gangrene
Progressive bacterial synergistic gangrene
Gas gangrene
Necrotizing cellulites
Necrotizing fasciitis
Necrotizing myositis
Myonecrosis
Clostridial myonecrosis
Clostridial cellulitis
Streptococcal myositis
Fournier’s gangrene
RISK FACTORS AND ETIOLOGY
Risk Factors
Although multiple risk factors for necrotizing soft tissue infections have been described, there are no studies specifically addressing this issue. Risk factors listed in the literature include: advanced age, diabetes mellitus, obesity, alcohol-use, intravenous drug use (IVDU), malnutrition, immune suppression, peripheral vascular disease, steroid use, and NSAIDs among others. These should be interpreted as conditions that have been associated with necrotizing soft tissue infections but lack data to support them as predictive of necrotizing soft tissue infections occurrence. Furthermore reports from different studies could be representing different population of patients with unequal characteristics. For example, in the study published by Wall et al, in which 31 patients with necrotizing soft tissue infections were compared to 328 patients with non-necrotizing soft tissue infections, no specific conditions were found to be predictive of necrotizing soft tissue infections, except for intravenous drug use as an etiologic factor (and possibly risk factor too). However this population of patients had a very high representation of intravenous drug use (71%) as compared to other series. On the other hand, a more recent study also comparing patients with necrotizing soft tissue infections (n=89) with those with non-necrotizing soft tissue infections (n=225) showed that the former were more likely to have comorbidities and were more commonly associated with the presence of DM (70% vs. 51%, no p value provided). Although no other studies comparing necrotizing soft tissue infections with non-necrotizing soft tissue infections have been identified, and establishing risk factors for necrotizing soft tissue infections remains difficult, multiple large series have reported what appeared to be meaningful associations between necrotizing soft tissue infections and the presence of chronic comorbidities, particularly the presence of diabetes mellitus and obesity (30-97% range). It remains unclear whether these are true risk factors for necrotizing soft tissue infections, but it is prudent to have a high index of suspicion in patients with chronic and debilitating comorbidities (DM, obesity, immune suppression, etc) who present with clinical or laboratory findings suggestive of necrotizing soft tissue infections.
NSAIDs have previously been described as risk factors and even causative factors for necrotizing soft tissue infections. However subsequent studies have failed to find significant relation between the use of NSAIDs and necrotizing soft tissue infections. Their use can certainly mask the initial symptoms from an ongoing soft tissue infection that can eventually progress towards necrotizing soft tissue infections, but true necrotizing soft tissue infections will probably progress regardless of the use of NSAIDs and good clinical judgment will be the key to early diagnosis and treatment.
Etiology
There are many events that can serve as etiologic factors to necrotizing soft
tissue infections. Some of the
published ones include: injection, trauma (lacerations, abrasions, wounds,
etc.), insect bites, chronic wounds/ulcers, postoperative infections, perirectal
abscesses, progression of minor soft tissue infections (furuncles, abscesses),
etc. Two main points deserve emphasis regarding the etiology of necrotizing soft
tissue infections. First,
idiopathic necrotizing soft tissue infections (those occurring in previously healthy patients without an
obvious source) constitute up to 20% of causes in major series, making a high
level of suspicion a key factor in diagnosing the disease in patients that may
not have a typical history leading to it. These patients have a
higher incidence of GAS related necrotizing soft tissue infections and infections more commonly compromise the
extremities. Secondly, patients that are intravenous drug use are definitely at an increased
risk of developing necrotizing soft tissue infections. Intravenous drug use is the route of entry and cause of infection in
7-56% of recent series and has its own features worth mentioning ![]() .
.
Intravenous Drug Use-Related Necrotizing Soft Tissue Infection.
Bosshardt, et al published a series of patients with predominantly intravenous drug use-related necrotizing soft tissue infections over a 5-year period and showed that the incidence more than doubled when compared to the first years of the study. These infections seem to be particularly associated with subcutaneous and muscle injection (skin popping/muscling) of “black-tar heroin”, a cheaper, dark and gummy form of heroin that is usually mixed with diluents like dirt or coffee allowing for bacterial spores to be introduced. Most of these infections are polymicrobial but a high prevalence of anaerobic bacteria including clostridium species has been reported, which explains the high white blood cell counts associated with it as well as its rapid progression and high mortality rate, in the order of 45%. Intravenous drug use patients should be considered as a high-risk group for developing necrotizing soft tissue infections and when evaluated for soft tissue infections should undergo a thorough assessment that can confidently rule out a necrotizing infection. Admissions of multiple intravenous drug use patients with necrotizing soft tissue infections in a short interval should raise the concern for an outbreak from a “bad lot of heroin” as has previously been described in the United Kingdom and in California.
MICROBIOLOGY
Necrotizing soft tissue infections are typically polymicrobial in nature. Some of the largest series evaluating the microbiology of necrotizing soft tissue infections showed that 84-85% of necrotizing soft tissue infections were polymicrobial in nature. Of these, the most common microorganisms isolated vary according to patient population, however in most series the three most common isolates are anaerobic bacteria (primarily bacteroides, Gram positive cocci and clostridium), staphylococcus and streptococcus species. Other less common reported isolates include Enterobacteriaceae, fungal species and specifically Mucormycosis and Vibrio species, both of which usually occur in immune suppressed hosts and carry an elevated mortality in the order of 40-80%. Table 5 lists the most common isolates from one of the largest series evaluating microbiology patterns of necrotizing soft tissue infections.
Table 5. Isolated Microorganisms and Type of Infections from Patients with Necrotizing Soft Tissue Infections in a Series of 182 Patients
| MICROORGANISM |
No. of isolates (n=791 isolates) |
| Anaerobes |
263 |
| Bacteroides/Prevotella spp |
136 |
| Peptostreptococcus |
49 |
| Clostridium |
37 |
| Streptococcus species (including enterococcus) |
236 |
| Groups A β-hemolytic |
57 |
| Staphylococcus species |
77 |
| Other (including other Gram positives, Gram negatives and fungi) |
215 |
| TYPE OF INFECTION |
Number of patients (n=182) |
| Polymicrobial infection |
154 (85%) |
| Monomicrobial infection |
28 (15%) |
| Group A β-hemolytic streptococcus |
15 (54%) |
| Clostridium species |
4 (15%) |
| Other |
9 (31%) |
Monomicrobial infections are less common presenting in approximately 14-15% of cases from major series. The most common isolates include Group A beta-hemolytic Streptococcal pyogenes (GAS), clostridial infections and more recently staphylococcus species. Series with larger representation of these isolates typically have a higher percentage of monomicrobial infections. Recent reports indicate that community acquired methicillin Staphylococcus aureus (CA-MRSA) can cause necrotizing soft tissue infections as a sole pathogen something that was extremely rare in the past.
Two specific infections are worth mentioning in more detail, those caused by GAS
and those caused by clostridial species. They share some similarities including
their unique ability to infect all the different compartments of the soft
tissues including subcutaneous tissue, the fascial layers and/or the muscle
compartments (myonecrosis/myositis). Although they are usually part of
polymicrobial isolates, both have been reported as the most common causes of
monomicrobial infections. They also cause a rapidly progressive, severe form of
necrotizing soft tissue infections mediated through exotoxins in the case of clostridial infections and
through cell wall components (M-protein) and exotoxins (streptococcal pyrogenic
exotoxins –SPE A, B and C-) in GAS infections. Their clinical manifestations are
secondary to the infectious process itself (local and systemic changes) as well
as to the effect from the different toxins released at the infection site (toxic
shock syndrome for clostridial infections and streptococcal toxic shock syndrome for GAS infections
![]() and the potential for directed therapies is valid for
both types of infections.
and the potential for directed therapies is valid for
both types of infections.
|
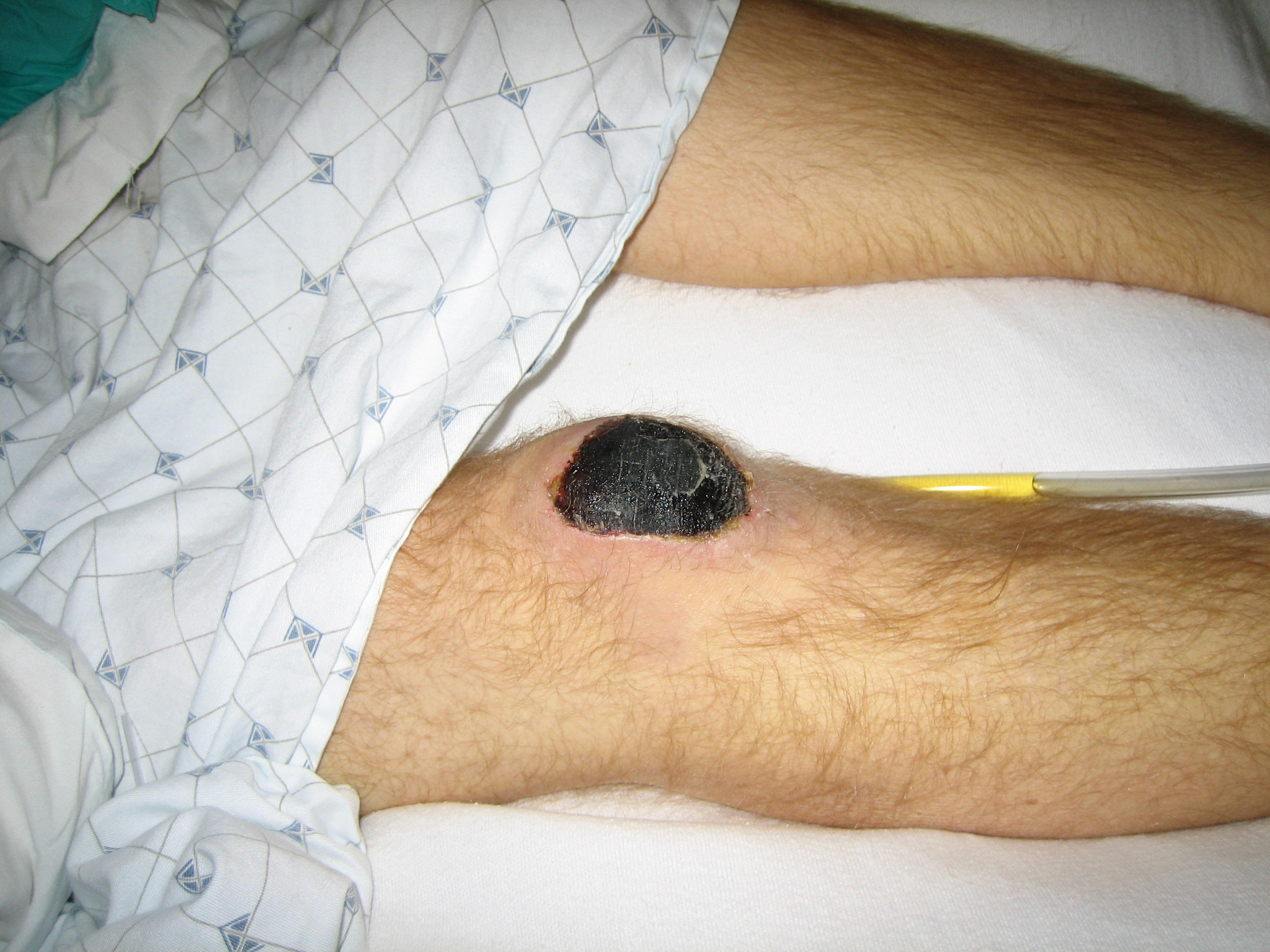
Peripheral ischemia associated with Streptococcus pyogenes toxic shock syndrome |
||||||
|
|
|
 |
 |
 |
||
|
34 year old male with rash associated with Streptococcus pyogenes toxic shock syndrome |
||||||
|
|
 |
|
||||
In a recent study by Anaya et al, clostridial infections were associated with increased risk of mortality and limb loss when compared to other non-clostridial necrotizing soft tissue infections (38% vs. 12% for mortality and 45% vs 19.5% for limb loss, respectively). In the same study, the authors evaluated the clinical differences between these two types of infections and showed that clostridial infections are more likely to be associated with intravenous drug use, present with significantly higher admission WBC counts, are more likely to be monomicrobial in nature, and have a more severe course as seen by higher APACHE II scores and worse outcomes. These findings have been reproduced in other studies of clostridial necrotizing soft tissue infections). Similarly, in a review of the cases of GAS-related necrotizing soft tissue infections in Ontario, Canada over a 4-year period, a similar mortality rate was seen to that of necrotizing soft tissue infections in general (34%), however when they were associated with streptococcal toxic shock syndrome (47% of the times), mortality increased significantly to 67%. Other predictors of mortality were advanced age, bacteremia, and hypotension. The use of clindamycin as well as intravenous immunoglobulin (IV Ig) was shown to be protective. The use of intraoperative Gram stain (predominance of Gram positive cocci) as well as the clinical course before and after debridement are tools that can help in guiding if these microorganisms can the causative factors for each specific infection, and if so consideration of directed therapies should be discussed.