Table 1. Organisms Associated with Nosocomial Catheter-Related Blood Stream Infections (CR-BSI).
|
Organism |
Comments |
|
Most common pathogen in CR-BSI |
|
|
Increasing prevalence of MRSA strains |
|
|
Gram-negative bacilli |
Among the resistant gram negative bacilli, Acinetobacter baumannii predominates in Europe. In USA Pseudomonas aeruginosa seems to be more prevalent |
|
E. faecalis is more common than e. faecium |
|
|
C. albicans is the most common species |
|
|
Other bacteria including diphteroids, viridans streptococci, Micrococcus, and more rarely, fungi other than Candida spp. |
|
The organisms are listed in order of
decreasing frequency. From multiple sources
(6, 9,11, 20, 21)
Table 2: Risk Factors for Bacteremia
|
· Advanced age · Corticosteroids · Immunosuppressing medications (transplant patients, rheumatologic diseases, etc) · Chronic liver disease · Chronic renal failure (especially if on hemodialysis) · Hematological malignancies · HIV infection · Intravenous catheters · Intravenous drug use · Loss of skin integrity · Malnutrition and hypoalbuminemia · Neutropenia · Parenteral nutrition |
Table 3. Contamination versus True Infection Rates for Specific Organisms.
|
Organism |
False positives |
|
Bacillus spp. |
>90% |
|
Coag-negative Staphylococcus spp. |
>90% |
|
Propionibacterium spp. |
>90% |
|
Corynebacterium spp. |
>80% |
|
Viridans streptococci |
50% |
|
Clostridium spp. |
40% |
|
Staphylococcus aureus spp. |
25% |
|
Enterococcus spp. |
15% |
Source. From a presentation by Dr. Patric Murray, University of Maryland School of Medicine.
Microbiology for the Millennium Conference. Feb. 17-19, 1999. Baltimore, MD
Table 4.
Organisms Causing
Nosocomial Blood Stream Infections by Frequency.
|
Organism |
Percent of BSI |
|
Coagulase-negative Staphylococcal spp. |
31.3% |
|
Staphylococcus aureus |
20.2% |
|
Enterococcus spp. |
9.4% |
|
Candida spp. |
9.0% |
|
Escherichia coli |
5.6% |
|
Klebsiella spp. |
4.8% |
|
Pseudomonas aeruginosa |
4.3% |
|
Enterobacter spp. |
3.9% |
|
Serratia spp. |
1.7% |
|
Acinetobacter baumannii |
1.3% |
Reference [11]
Table 5. Risk Factors for Infective Endocarditis
|
Non-cardiac |
Cardiac |
|
· IV drug abuse · Male · Advancing age · Recent dental surgery or other invasive procedures · Nosocomial bacteremia · Permanent venous access lines · Surgically constructed pulmonary shunts |
· Degenerative valvular lesions · Congenital heart disease · Prosthetic valves · Mitral valve prolapse with insufficiency · Rheumatic heart disease · Previous infective endocarditis · Hypertrophic cardiomyopathy |
Table 6: Risk Factors for Gram Negative Bacilli Bacteremia
|
Table 7. Characteristics of the Major Candida spp.
|
Species |
Frequency |
Virulence |
Clinical Associations |
|
42% - 65% |
High |
Most common in all settings |
|
|
11% - 25% |
High |
Cancer |
|
|
7% - 15% |
Low |
Cancer |
|
|
7% - 18% |
Variable |
Plastic devices, hyperalimentation |
|
|
1% - 4% |
Low |
Cancer |
|
|
C. lusitaniae |
1% - 2% |
Low |
Cancer |
Shown are frequency estimates for the species causing invasive disease.
Table 8. Primary and Alternative Empiric Antibiotic Choices for Bacteremia
|
|
Primary |
Alternative |
|
Gram-positive cocci in clusters* |
Vancomycin OR daptomycin^ |
Nafcillin OR cefazolin (once MRSA ruled out)
|
|
Gram-positive cocci in chains |
Ampicillin OR vancomycin |
Ceftriaxone** OR daptomycin
|
|
Gram-negative bacilli in a clinically unstable patient, immunosupressed, history of malignancy or a patient with health care associated infection
|
Cefepime + ciprofloxacin (or tobramycin) OR piperacillin/tazobactam + ciprofloxacin (or tobramycin) |
Aztreonam + tobramycin (or ciprofloxacin OR imipenem + ciprofloxacin (or tobramycin) |
|
Gram-negative bacilli in a clinically stable patient
|
Ceftriaxone OR piperacillin/tazobactam |
Aztreonam OR ciprofloxacin |
|
Anaerobes |
Piperacillin/tazobactam OR metronidazole
|
Clindamycin OR Imipenem |
|
Candida sp. |
Echinocandin OR voriconazole |
^daptomycin not indicated if patient clinically has pneumonia.
*consider the addition of a second agent such as gentamicin if patient is clinically unstable or endocarditis is likely
**Do not use if enterococcus is a potential cause of infection
“May be used as a first line agent when patient is hemodynamically stable and no previous azoles administered
Figure 1: Staphylococcal spp. are Always Catalase Positive while Streptococcal spp. are Catalase Negative
Figure 2: Classification of Gram Negative Bacilli
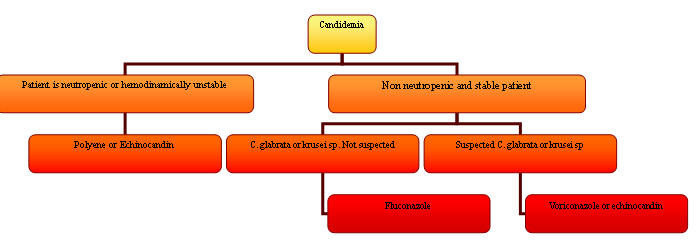
Figure 3. Algorithm for the Treatment of Candidemia