Chronic Sinusitis
Authors: Berrylin J. Ferguson, M.D.
DEFINITION
Chronic sinusitis has traditionally been attributed to unresolved or improperly treated acute disease. In recent years, it has become apparent that a variety of causes and associations are present in the inflammatory condition of CRS. In 1996, a task force convened by the American Academy of Otolaryngology Head and Neck Surgery published definitions of sinusitis and termed the entity "rhinosinusitis" in order to emphasize the relationship of nasal symptoms and nasal pathology to sinus disease (3). Subsequently, in 2004, these definitions were expanded, based on consensus of experts from allergy-immunology, rhinology, infectious disease and radiology (5). The currently accepted definition of chronic rhinosinusitis (CRS) is inflammation of the nose and paranasal sinuses with objective evidence of disease by radiographs or nasal endoscopy and with a duration of symptoms and signs of at least 12 weeks. In the lengthy document generated supporting this definition of CRS, evidence supporting a variety of etiologies, some of which are well defined and some of which are theoretical is reviewed. In fact several mechanisms are probably acting concurrently in some patients.
EPIDEMIOLOGY
Chronic rhinosinusitis (CRS) is a diverse group of disorders. The perceived prevalence exceeds the actual prevalence, nevertheless it is common and over 500,000 endoscopic sinus surgeries are performed each year for this indication. Notably, half of patients who complain of CRS symptoms have no objective evidence of disease, either endoscopically or by radiographs (12). Within these caveats, it is true that the diagnosis is increasing in prevalence and estimated to affect approximately 31 million Americans a year.
Chronic rhinosinusitis is now commonly subdivided into CRS with nasal polyps (NP) or CRS without nasal polyps. Each of these categorizations is discussed separately under pathogenesis and clinical manifestations. While there is overlap between these two classifications, this categorization provides a simple mechanism of stratifying patients, recommending therapies and providing prognosis. The incidence of nasal polyps is between 0.2 to 4% of the population, and increases with age, peaking at age 50 years or greater. A familial history is reported in 14% of patients. Commonly associated conditions include asthma, particularly those with adult onset asthma and aspirin sensitivity, ciliary dyskinesia syndromes (Kartagener’s syndrome/Young’s syndrome), cystic fibrosis, Churg-Strauss syndrome, allergic fungal sinusitis and bacterial rhinosinusitis. The latter two associations are frequently unilateral (Table 1). The most refractory of the CRS patients with nasal polyps, have a histopathology characterized by eosinophilia and eosinophilic mucin. These patients are also categorized as eosinophilic CRS (ECRS) an account for 80% of nasal polyp patients (Table 2)
Chronic rhinosinusitis without nasal polyps may encompass early forms or controlled forms of all the disorders associated with CRS with nasal polyps. In many patients with CRS without nasal polyps, the disease may be associated with structural abnormalities causing obstruction of the outflow tract of the maxillary and ethmoid sinuses. In these patients, surgery directed at the limited area of obstruction restores function to the sinuses and is termed functional endoscopic sinus surgery (FESS). Surgery in these cases may also be successful because it mechanically debrides away biofilms. Patients may develop this disorder after a repeated or prolonged bacterial infection that causes irreversible mucosal thickening or osteoneogenesis, causing an obstruction of the osteomeatal complex. In addition medically refractory CRS reflects immunodeficiency, allergy and exposure to environmental insults. Up to half of patients with medically refractory sinusitis in one retrospective review, had an immunodeficiency including low immunoglobulin levels and impaired cellular function. Prior to the advent of effective antiretroviral therapy for human immunodeficiency virus (HIV) disease, CRS was a common finding in the HIV-positive patient, even before the appearance of the clinical manifestation of the acquired immunodeficiency syndrome (AIDS).
Atrophic rhinitis is a dry crusty nasal condition in which the lining of the nose is colonized and infected with bacteria. Rhinoscleroma ozenea is the usual pathogen in this unusual infection which is much more commonly seen in the underdeveloped countries and in impoverished conditions.
Recurrent acute rhinosinusitis is different from chronic persistent rhinosinusitis. Recurrent sinus infections are considered to fall outside normative patterns, if more than 3 distinct episodes occur a year. A common scenario accounting for this pattern is a parent with young children who attend daycare. In the absence of exposure to sick children, investigations of allergy and immunodeficiency are appropriate.
Acute exacerbations of CRS are commonly seen in patients who have already had one or many prior sinus surgeries. These episodes may represent viral, bacterial or non infectious exacerbations of their disease. The organisms cultured in these patients are Staphylococcus aureus, Pseudomonas aeruginosa, and acute pathogens such as Streptococcus pneumoniae and Haemophilus influenza.
PATHOGENESIS AND CLINICAL MANIFESTATIONS OF BACTERIAL CRS
Pathogenesis of Chronic Bacterial Sinusitis
Most cases of CRS are inflammatory with only a questionable relationship to traditional bacterial infectious etiologies. Nevertheless, CRS is one of the most common diagnoses for which outpatient antimicrobial therapy is prescribed. There are no blinded controlled studies to date demonstrating efficacy of oral or systemic antimicrobials in chronic rhinosinusitis. Patients with unilateral disease, without nasal polyps are most likely to represent chronic bacterial infectious sinusitis. Anaerobes play a controversial role in CRS; however both anaerobic and aerobic cultures should be obtained if the diagnosis is suspected. One postulated cause of bacterial persistence is the formation of bacterial or mixed bacterial/fungal biofilms. Biofilms have recently been demonstrated in CRS (1, 2). A bacterial biofilm is relatively resistant to antimicrobial therapy and may demonstrate sensitivity to antimicrobials by culture of the planktonic form, not present in the biofilm form. The most effective treatment of a biofilm is mechanical debridement, either with surgery of with vigorous nasal irrigations, particularly if prior sinus surgery has made the sinus cavities accessible to nasal irrigation. In the presence of long standing disease, osteoneogenesis can be seen thickening the sinus walls radiographically. Whether this is secondary to bacterial infection or other inflammatory causes is unclear (Figure 1). Histopathologically, patients with chronic bacterial sinusitis will often show a neutrophilic or lymphocytic infiltrate. The microbial flora of patients with prior surgery is complex and no definite relationship exists between therapy directed at these microbes and resolution of disease. Nevertheless it is common to have the patient use antimicrobial washes based on the sensitivities of the organisms cultured endoscopically.
Structural and anatomic factors in the early days of endoscopic sinus surgery were felt to be the major cause of CRS. We now recognize that structural factors are just one cause of many. The term ostiomeatal complex describes the physiologic arrangement of the structures into which the maxillary and anterior ethmoid and frontal sinuses’ mucociliary action is directed and through which they are ventilated and drain. Obstruction in the ostiomeatal complex can lead to disease in these dependent sinuses (Figure 2 and 3). In these situations, endocscopic sinus surgery limited to the area of obstruction can result in restoration of function of the sinuses. In situations where the surgery restores function to the sinuses the term functional endoscopic sinus surgery (FESS) is frequent used. Obstruction in the area the ostiomeatal complex may develop after a prolonged or repeated infection which can lead to irreversible mucosal hypertrophy or osteoneogenesis which then blocks the outflow tracts of the draining sinuses.
Maxillary dental infections can cause bacterial maxillary sinusitis. The pathogens are mixed and include anaerobes.
Diagnosis
Physical Examination
The most common finding in patients with chronic bacterial rhinosinusitis is nasal congestion, upper teeth pain on the side of the afflicted maxillary sinus, facial pain or pressure and purulent discharge. Nasal congestion can exist without concomitant sinusitis. Having the patient blow the nasal secretions into a tissue for examination allows one to assess the material for purulence. An otoscope may be useful in anterior rhinoscopy. Ideally nasal endoscopy can be performed. This allows evaluation of the middle meatus and the outflow tracts of the various sinuses. The nasopharynx can be assessed for adenoidal hypertrophy or masses which can mimic nasal congestion. In addition endoscopically guided cultures of purulence can be obtained. Nasal polyps may be visualized and have the appearance of peeled grapes. They must be distinguished from the inferior and middle turbinates which may also have a pale and boggy appearance.
Nasal polyps may be associated with chronic bacterial sinusitis, but generally they are restricted to the side of the infection.
Infectious complications of sinusitis, are more common with acute than chronic infections (6). If the frontal sinus is infected it may eventually cause an osteomyelitis of the anterior or posterior table. If the anterior table of the frontal sinus is involved then one develops pain and fluctuance over the frontal sinus and may eventually develop a sinus fistula with drainage of purulence. This is termed Pott's puffy tumor ( Figure 4 and 5).
Microbiologic Testing
The gold standard for the diagnosis of an infectious agent in sinusitis is an antral tap of the maxillary sinus or the recovery of tissue from an infected sinus surgically. Recently endoscopically guided cultures have gained increased acceptance as a moderately good surrogate for invasive diagnostic procedures. Endoscopically guided cultures have a correlation of 50 to 75% with antral taps. In CRS the role of bacteria is problematic. Most clinicians consider heavy growth of bacteria to be clinically significant. The role of anaerobic infections in chronic rhinosinusitis is controversial with the literature reporting isolation of anaerobes in 0 to 100% of cases of CRS. It is clear that S. aureus and Gram negatives such as Pseudomonas are isolated in dramatically more cases in CRS than in acute rhinosinusitis. Whether these bacteria are pathogenic or merely colonizers of irreversibly diseased mucosa may vary with the patient and the circumstance. Well over 50% of patients with nasal polyps will grow S. aureus from their polyps. The most common organism reported in large studies is coagulase negative staphylococci; however, coagulase negative staphylococci is found even more commonly in normal and is usually discounted as a pathogen. Streptococcus viridans and alpha hemolytic strep are usually considered nonpathogenic.
The presence of organisms on a gram stain is an indication of moderate quantity of bacteria. Unfortunately the description of presence of white blood cells is frequently not helpful in CRS because many of these cases are rich in eosinophils regardless of infection and the microbiology lab is unable to differentiate the eosinophil from the neutrophil on the gram stain. The in vitro sensitivities present by microbiologic testing allow direction of the antimicrobial agent to that most specific to the organism.
Microbiology of Bacterial Complications of Acute and Chronic Rhinosinusitis
The most common organisms isolated from all sinogenic intracranial complications are S. aureus and S. epidermidis, aerobic and anaerobic streptococcus species, although a wide variety of anaerobes, Gram negative bacteria, and even Actinomycetes have been reported. The most common organism isolated from both ocular and intracranial sinogenic complications in children from one institution, was Streptococcus milleri. The S. milleri group includes three species: S. intermedius, S. constellatus, and S. anginosus, which are commensal organisms present in the oral cavity, gastrointestinal tract, and urogenital system. Unlike other viridans Streptococci, the S. milleri group often is associated with abscess formation. Identification to the species level is difficult and is often unreliable with commercial laboratory kits. On blood agar, S. milleri organisms may be α-hemolytic, β-hemolytic, or nonhemolytic (6).
PATHOGENESIS AND CLINICAL MANIFESTATIONS: Eosinophilic CRS, Usually Associated with Nasal Polyps
While ostio- meatal obstruction is a commonly postulated mechanism for chronic and recurrent bacterial sinusitis, it appears to have little to no role in patients with diffuse sinus disease or with eosinophilic mucin plugs. Rather these patients suffer from a variety of as yet incompletely understood immunologic dysregulations which lead to a clinical picture characterized by eosinophilic mucin, nasal polyps and frequent association with eosinophilic inflammation of the lower airways, usually diagnosed as asthma.
Clinical Manifestations
Most of these patients have nasal polyps and sticky glue like green mucus. While yellow mucous is associated with viral/bacterial infections, the translucent green mucous in these patients reflects the high eosinophil counts and may or may not be associated with infectious agents. These patients, as with most patients with nasal polyps frequently have absent or impaired sense of smell. Congestion and thickened discolored secretions are common. Facial pain and pressure is less common in these patients then in patients with acute disease or non polypoid disease. Many of these patients have asthma.
Radiographic Findings
Radiographs in patients with asthma with or without nasal polyps are frequently positive, even when the patient is asymptomatic with regard to sino-nasal symptoms. A positive radiograph in an asthmatic, including one demonstrating pansinusitis, is hardly ever an emergency, and usually reflects the baseline findings. Close clinical integration of the patient’s time course of symptoms and any clinically localizing symptoms, with the radiographs is required. Diagnosis is facilitated with endoscopic visualization and endoscopically directed cultures and biopsies if indicated. Radiographs in patients with eosinophilic mucin often show a “white out” of the sinuses. A difference in density within the sinuses represents the presence of mucin plugs within the sinus surrounded by the less dense thickened mucosal lining of the sinus (Figure 6). This double density is also seen in Allergic Fungal Sinusitis. Bony erosion of the skull base or orbit is present in up to 20% of cases and does not indicate fungal invasion (Figure 7).
Diagnosis
Physical Examination in Eosinophilic CRS and with Nasal Polyps
While nasal endoscopy may be required to visualize nasal polyps which are small or restricted to the sphenoid recess and nasopharynx, large obstructing polyps can be visualized with lighted examination of the anterior nose. The polyps are usually smooth and a light pink to slightly yellow color and may be so large on rare occasions as to completely obstruct the front of the nose.
Sticky green mucin plugs are characteristic of eosinophilic rhinosinusitis. In massive nasal polyposis or in subcategories of CRS such as allergic fungal sinusitis (AFS), a remodeling of the facial skeleton may occur and hypertelorism or proptosis may be present. A mucocele (a dilated sinus filled with mucus because it is unable to empty into the nasal cavity) may cause double vision by eroding into the orbit.
Microbiology
The mucin plugs can be submitted for gram stain, fungal, anaerobic and aerobic culture. Anaerobic cultures are seldom submitted in this setting unless the specimen is retrieved anaerobically from the sinuses during a surgical procedure. Microbiologic results are not always concordant with pathology. That is fungi may be seen on pathology of the mucin plugs and not grow from culture. The opposite is true as well and findings must be integrated into the clinical context.
As many as 60% of patients with eosinophilic mucin plugs have bacteria present by staining. The significance of this is not clear. These stains do not necessarily correlate with results from cultures. Over 50% of nasal polyp patients are colonized with S. aureus. The role this plays in the disease is also unclear but may be important in superantigen mediated inflammation (discussed below). Cultures are important, if one is treating with antibiotics, since methicillin resistant S. aureus is increasingly common. Empirically community acquired MRSA is still sensitive to doxiciclin. Whether antimicrobial therapy has a role in this setting is unclear.
Theoretical Categorizations of Eosinophilic Chronic Rhinosinusitis
Within the category of eosinophilic CRS, lie several possible mechanisms of disease. These include superantigen mediated, which is believed to be a result of upregulation of inflammation by exotoxins produced by S. aureus (9,10). Over half of nasal polyp patients will demonstrate a moderate to heavy growth of S. aureus. To date, no studies have been performed that show that antimicrobial therapy is efficaccious in this scenario. Other suggested etiologies of eosinophilic CRS include Aspirin Exacerbated Eosinophilic Chronic Rhinosinusitis, Allergic Fungal Sinusitis and nonallergic fungal eosinophilic chronic rhinosinusitis (Table 2).
Aspirin exacerbated CRS is also known as Aspirin Exacerbated Respiratory Disease (AERD), aspirin intolerant asthma or Samter’s triad. This grouping associated with an adverse reaction to aspirin is usually typified as an asthma attack, is present in about 5 % of all asthmatics. The syndrome characteristically presents after age 40. Whether a viral event initiates this hypersensitivity is unknown. Currently the relationship of the development of aspirin sensitivity to superantigens is under investigation. Ingestion of aspirin or nonsteroidal anti-inflammatory agents provokes nasal congestion and bronchoconstriction (4).
Allergic fungal sinusitis may present in children or adults and may be unilateral or bilateral. The diagnosis depends on detecting hyphae in the eosinophilic mucin extracted from the nose and sinuses. Classically, patients also demonstrate an elevated IgE to the cultured fungus and frequently to many molds and pollens (4). Anecdotally systemic and topical antifungals have been helpful; however randomized controlled trials to date have failed to show significant benefit. In the pulmonary correlate of allergic fungal sinusitis, which is allergic bronchopulmonary aspergillosis (ABPA), itraconazole has been shown to be effective (13). Immunotherapy directed toward molds may be helpful postoperatively but not prior to surgical extraction of the disease. Recurrence is common and steroids are the mainstay of therapy (4).
Nonallergic fungal eosinophilic chronic rhinosinusitis is an entity popularized by Jens Ponikauand colleagues (7). These investigators have demonstrated that fungi can be cultured from almost anyone's nose whether afflicted with chronic rhinosinusitis or not. They have also suggested that Alternaria can induce an inflammatory reaction in the peripheral blood monocytes of patients with CRS but not normal controls (11). In one small pilot study they showed that there was an 8% reduction in mucosal thickening by sinus CT scan after four months of twice daily irrigation with amphotericin B; however, there was the significant difference in symptoms in patients treated with amphotericin B and those receiving irrigation with the placebo. Other investigators in randomized controlled trials have demonstrated no difference in patients treated with topical antifungals.
Steroids are the main stay of therapy, as in all eosinophilic CRS patients, both topically for control of disease and systemically for flares.
PATHOGENESIS AND CLINICAL MANIFESTATIONS OF SYSTEMIC DISEASE MANIFESTING WITH NASAL DISORDERS
Systemic disorders such as pemphigoid, sarcoidosis, Wegener's granulomatosis and various vasculitidies can present with refractory rhinosinusitis. Cocaine abuse can present a clinical picture very similar to vasculitis, almost always associated with a septal perforation and is a diagnosis based on exclusion of vasculitis. On top of the diseased and impaired mucosa associated with these disorders, secondary bacterial infection is common (Table 2).
Clinical Manifestations and Physical Examination
Bleeding, scarring and crusting of the lining of the nose extending beyond the most anterior segment is suspicious for the diagnosis of Wegener's granulomatosis or hereditary telangectasia. Sarcoidosis produces a cobblestone like appearance to the nasal septum and turbinates. Examination of the oropharynx may reveal thickened white or discolored drainage. Cicatricial pemphigoid is associated with scarring and narrowing of the nasal vestibule and nasal cavity even to the extent of complete obstruction.
Radiography
In systemic disease, septal perforation particularly with disorders associated with vasculitis is common. The lining of the nasal cavity is also frequently thickened. These findings are however non specific for systemic disease.
Laboratory Testing
Patients whose nasal mucosa is chronically crusted or cobblestoned in appearance should be evaluated for Wegener's granulomatosis and sarcoidosis. The suggested laboratory evaluation for Wegener's granulomatosis includes a cANCA and sedimentation rate. An angiotensin converting enzyme level may be half helpful in the diagnosis of sarcoidosis.
Laboratory Testing for Bacterial and Eosinophilic CRS
From 50 to 80% of patients with sufficient symptoms to require surgery have allergies, which are usually perennial. This includes all categories of CRS. Allergy testing may be done with blood tests for specific IgE's for a panel of antigens or with skin testing, either prick testing or intradermal testing. A suggested in vitro screening for allergies is listed in Table 3. A total IgE is not an adequate screen for allergies since it may be normal even in the presence of significant allergy. In the entity allergic fungal sinusitis, total IgE is frequently elevated, as well as elevated specific IgE's to fungi, particularly dematiaceous fungi such as Alternaria, Curvularia and Bipolaris. Serum eosinophilia is common in allergic fungal sinusitis and nasal polyps and is associated with refractory and recurrent disease.
Immunodeficiency
In patients with recurrent acute sinusitis (three or more discreet episodes of < eight weeks) or medically refractory disease, the differential diagnosis includes immunodeficiency. A screening immunodeficiency workup is listed in Table 4.
Imaging
The most useful test for imaging the paranasal sinuses is a coronal sinus CT scan. With high-speed serial sinus CT the radiation dosage is < or equivalent to a full panel sinus series and delivers much greater information. Incidental findings on sinus CT and without clinical significance are common. Rounded retention cysts in the sinuses are usually nonpathologic. Patients with asthma, even with minimal sinus symptoms, frequently have mucosal thickening of all or most of their sinuses (Figure 2). This common finding must be considered in determining the significance of the positive sinus CT scan in an asthmatic. The CT scan is most helpful when the findings of disease correlate with the patient’s symptomatology. In addition a completely negative sinus CT scan is valuable in eliminating a sinus infection from the differential diagnosis. Because 80% of patients with a viral infection will have an abnormal sinus CT scan indistinguishable from the findings on a bacterial sinus infection, a sinus CT scan should only be obtained when the patient’s disease presentation is puzzling, or there is persistence of symptoms after maximal and directed medical therapy. A sinus CT should be obtained immediately in patients with orbital or potentially intracranial complications of sinusitis (6).
A Magnetic Resonance Image (MRI) of the sinuses is seldom as helpful as a CT scan. The MRI is far too sensitive to the findings of nasal congestion and also fails to adequately display the bony sinus walls. They magnetic resonance angiogram (MRA) is helpful in evaluation of cavernous sinus thrombosis.
EMPIRIC THERAPY prior to Definitive Diagnosis
In the vast majority of cases initial empiric therapy should include a nasal steroid spray. Nasal douching and saline washes are frequently employed. Because antimicrobial therapy in CRS, if indeed it is secondary to a bacterial agent, may well require a longer course of therapy than with acute disease, an endoscopically guided culture should be performed prior to initiating antimicrobial therapy. If antimicrobial therapy is initiated in the absence of a culture, one should expect clinical improvement within three to four days. In the absence of improvement one should suspect that the etiology is either nonbacterial or the bacteria are resistant to the antibiotic being administered. There are few randomized controlled trials in the literature studying antibiotics and chronic rhinosinusitis and none with a placebo control. Recently Lund and colleagues demonstrated that nasal douche, nasal steroid sprays, and three months treatment with a macrolide was as effective as sinus surgery in CRS (8). Macrolides have interesting anti-inflammatory effects akin to those of corticosteroids.
Efficacy of topical and sinus installation antibiotics and antifungals is uncertain. In a completed randomized placebo controlled study, patients with strict entry criteria of prior endoscopic sinus surgery in the presence of purulence were shown to have both objective and subjective improvement on daily nebulized tobramycin compared to placebo.
Intravenous antibiotic therapy may be helpful in patients with bacterial rhinosinusitis who have failed oral therapy. These interventions are frequently undertaken in immunocompromised patients such as double lung transplant cystic fibrosis patients. Ideally, the IV therapy is directed by sinus cultures and sensitivities. No controlled studies have documented the superiority of IV administration of antibiotic therapy in CRS. Topical antimicrobials may reduce symptoms and relapse and are outlined in Table 5.
References
1. Ferguson BJ. Categorization of eosinophilic chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2004;12:237-242. [PubMed]
2. Ferguson BJ, Stolz DB. Demonstration of biofilm in human bacterial chronic rhinosinusitis. Am J Rhinol. 2005;19(5):452-457. [PubMed]
3. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997; 117:S1-7. [PubMed]
4. Marple BF. Allergic fungal rhinosinusitis: current theories and management strategies. Laryngoscope. 2001;111:1006–1019. [PubMed]
5. Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114(6 Suppl):155-212. [PubMed]
6. Oxford LE, McClay J. Complications of acute sinusitis in children. Otolaryngol Head Neck Surg. 2005;133(1):32-37. [PubMed]
7. Ponikau JU, Sherris DA, Kern EB, et al. The diagnosis and incidence of allergic fungal sinusitis. Mayo Clin Proc. 1999;515:18–21. [PubMed]
8. Ragab SM, Lund VJ, Scadding G. Evaluation of the medical and surgical treatment of chronic rhinosinusitis: a prospective, randomized, controlled trial. Laryngoscope. 2004;114(5):923-930. [PubMed]
9. Schubert MS. A superantigen hypothesis for the pathogenesis of chronic hypertrophic rhinosinusitis, allergic fungal sinusitis, and related disorders. Ann Allergy Asthma Immunol. 2001; 87:181–188. [PubMed]
10. Seiberling KA, Conley DB, Tripathi A, et al. Superantigens and chronic rhinosinusitis: detection of staphylococcal exotoxins in nasal polyps. Laryngoscope. 2005;115(9):1580-1585. [PubMed]
11. Shin SH, Ponikau JU, Sherris DA, et al. Chronic rhinosinusitis: an enhanced immune response to ubiquitous airborne fungi. J Allergy Clin Immunol. 2004;114(6):1369-1375. [PubMed]
12. Stankiewicz JA, Chow JM. Nasal endoscopy and the definition and diagnosis of chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2002;126:623-627. [PubMed]
13. Stevens DA, Schwartz HJ, Lee JY, et al. A randomized trial of itraconazole in allergic bronchopulmonary aspergillosis. N Engl J Med. 2000;342:756–762.[PubMed]
Tables
Table 1: Some Pathophysiologic Factors Associated With CRS
Host |
Environmental |
|---|---|
Autoimmune disease |
Allergens |
Ciliary Dysfunction |
Bacteria |
Cystic Fibrosis |
Fungi |
Granulomatous Disorders |
Irritants/Pollutants |
Immunodeficiency |
Smoking |
Prior Sinus Surgery |
Stress Viruses |
Table 2: Pathogenesis-based Subclassification of ECRS with Therapeutic Interventions by Reported and Theoretical Efficacy
|
Proposed Mechanisms |
Steroids Systemic or Topical |
Immunotherapy |
Leukotriene Modulator |
Anti-Bacterials Systemic or Topical |
Anti-fungals Systemic or Topical |
Anti-IgE |
Aspirin Desensitization |
|---|---|---|---|---|---|---|---|---|
SAI– ECRS |
Superantigen upregulation from bacteria (staph) or other microorganisms, i.e. fungus |
+++ |
|
? |
?+ |
|
?+ |
|
AFS |
IgE mediated hypersensitivity to fungus growing in mucin |
+++ |
++ |
?+ |
|
++ |
?+ |
|
NAF-ECRS |
Non IgE mediated hypersensitivity to fungus in nose and mucin |
+++ |
|
?+ |
|
+ |
|
|
AE-ECRS |
Leukotriene overproduction |
+++ |
|
++ |
?+ |
|
? |
++ |
ECRS-Eosinophilic Chronic Rhinosinusitis SAI-ECRS-Superantigen Induced Eosinophilic Chronic Rhinosinusitis AFS -Allergen Fungal Sinusitis NAF-ECRS-Non-Allergic Fungal Eosinophilic Chronic Rhinosinusitis AE-ECRS-Aspirin Exacerbated Eosinophilic Chronic Rhinosinusitis
Table 3: Suggested Initial In Vitro Allergy Screen
| Dust mite (Der p 1 and Der f 1) |
| Cockroach |
| Cat |
| Dog |
| Alternaria |
| Cladosporium |
| Aspergillus |
| Timothy grass (or dominant regional grass) |
| Ragweed |
| 2 Tree pollens dominant in region |
Table 4: Initial Immunodeficiency Screen
| CBC with differential |
| If lymphopenia is noted, then obtain T cell subpopulations |
| IgG, IgG1, IgG2, IgG3, IgA, IgM, IgE |
| CH 50 (to screen for complement deficiency) |
| Pneumoccocal Titers (before and 6 weeks after pneumococcal vaccine) |
| Laboratory evaluation in Granulomatous Disorders |
| Wegener’s Granulomatosis: cANCA, sedimentation rate |
| Sarcoidosis: angiotensin converting enzyme
Both false negatives and false positives are possible |
Table 5: Dosages of Commonly Utilized Topical Antibacterials and Antifungals are Listed. None of These Have Been proven to be Efficacious.
Drug |
Concentration |
Dosage |
Targeted Organisms |
|---|---|---|---|
Amphotericin B. |
50 mg in 500 ml of water |
20 ml irrigation BID |
Fungi |
Gentamycin |
80 mg in 500 ml of saline |
10-20 ml irrigation QD to BID |
Pseudomonas |
Mupirocin ointment |
5 grams in 45 cc saline |
2 puffs BID to QID |
Staph aureus, strep pneumoniae, H. influenza |
Figure 1: Note Unilateral Maxillary Sinus Disease and Profound Maxillary Sinus Osteoneogenesis (arrow)

Figure 2: Note circle denotes Ostiomeatal complex
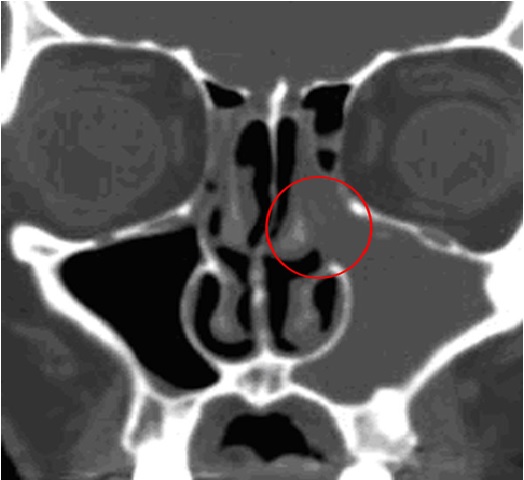
Figure 3: Note Arrows Indicating Mucociliary transport are oriented toward the ostium which is circled in yellow. Blockage of this ostium is believed to contribute to persistent bacterial infection.

Figure 4: Axial CT Showing Anterior and Posterior Frontal Sinus Erosion in "Pott's Puffy Tumor"
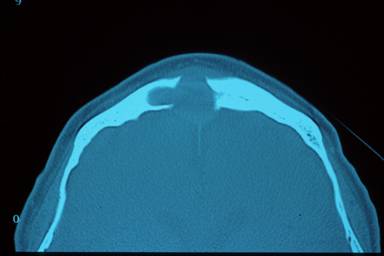
Figure 5: Pott’s Puffy Tumor (Osteomyleitis of the Anterior Table of the Frontal Sinus), Showing Sinus Draining out of Forehead

Figure 6: Coronal Sinus CT of Patient with Massive Obstructing Nasal Polyps and Eosinophilic Mucin Plugs (arrow), Note Lighter Color of Plug
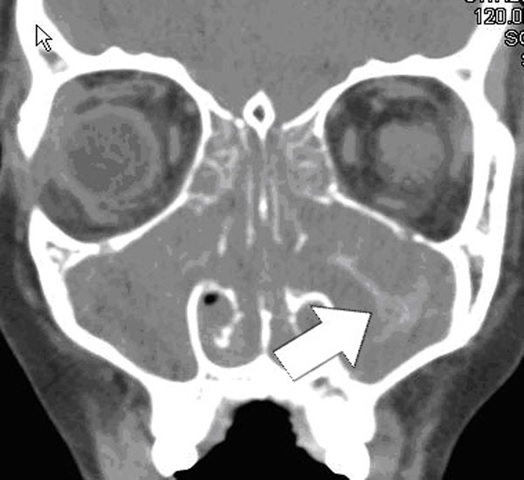
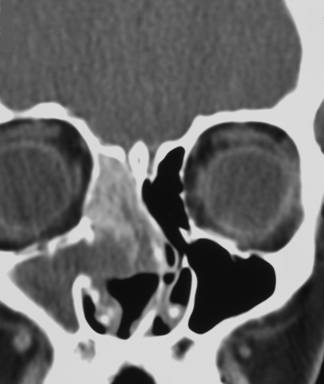
Figure 7: Coronal CT Showing Allergic Fungal Sinusitis in Right Ethmoid. The Patient has had Prior Surgery, Note Absence of Ethmoid Partitions and Uncinate. The Lighter Density Represents the Allergic Mucin Plug with the Fungal Presence, the Darker Density Represents Polypoid Changes.
What's New
Mandal R. Role of antibiotics in sinusitis. Curr Opin Infect Dis 2012 Apr;25(2):183-92
Guided Medline Search For:
Guided Medline Search For Recent Reviews
Guided Medline Search For Historical Aspects
Table of Contents
- Definition
- Epidemiology
- Pathogenesis and Clinical Manifestations of Bacterial CRS
- Pathogenesis and Clinical Manifestations: Eosinophilic CRS, Usually Associated with Nasal Polyps
- Pathogenesis and Clinical Manifestations of Systemic Disease Manifesting with Nasal Disorders
- Immunodeficiency
- Imaging
- Empiric Therapy Prior to Definitive Diagnosis

