


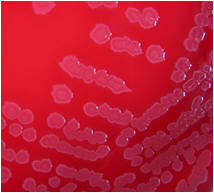
Numerous colony morphologies ( hemolytic & non-hemolytic)
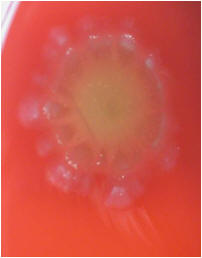
Beta hemolysis (β-hemolysis): Beta hemolysis is the complete lysis of the red blood cells around and under the colonies on a blood agar plate. This area appears transparent. Streptococcus pyogenes displays beta hemolysis and is often called Group A beta-hemolytic strep (GABHS).
Possible
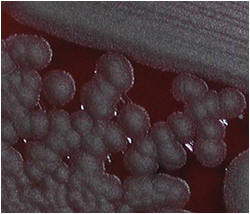
- Very fast growing
- Colony sticks together
- Non-motile
Major pathogen: Bacillus anthracis
Others only in immunocompromised patients from several blood cultures
@ Ellen Jo Baron 2007


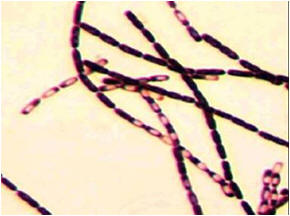



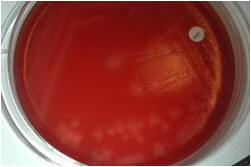

Regular Gram + rods & spores (do not stain)
from broth – central spores